This chapter describes changes in lifestyle behaviours and their impact on key risk factors associated with weight gain – i.e. unhealthy diets and physical inactivity. Trends in overweight and obesity and their subsequent impact on health and economic outcomes are also discussed. The chapter concludes with a summary of policies taken at both the national and international level to address this major public health issue.
Healthy Eating and Active Lifestyles

2. Overweight and its threat to public health
Abstract
Key messages
Changing environmental factors that dictate lifestyle behaviours have fuelled overweight, which disproportionality affects poorer populations
Factors such as advances in technology, globalisation, urbanisation and the expansion of food retail have changed the way people eat. Consequently, diets are increasingly comprised of foods associated with weight gain (e.g. added fats and sugar) at the expense of foods with healthy dietary elements (e.g. fruits and vegetables).
People today also have fewer reasons to be physically active (PA) with approximately one in three adults in OECD and the EU27 insufficiently active. In addition, levels of sedentary behaviour are high due to a variety of reasons such as the proliferation of labour-saving technologies: in the EU, nearly four in ten adults complete their work sitting down.
It is widely recognised that an imbalance between energy intake from food and energy expenditure from PA drives individual weight loss/gain. Therefore, it is not surprising that today more than half of all adults in the OECD live with overweight, with rates higher among those with a low socio‑economic status.
Overweight has a heavy toll on both health and economic outcomes
Those living with overweight are at greater risk of developing certain NCDs in adulthood such as type 2 diabetes, however, health effects also occur at an early age such as difficulties breathing. Overweight also depresses workforce productivity due to increases in absenteeism and presenteeism. Modelling work by OECD estimates that member countries spend 8.4% of their health budget to provide treatment for overweight‑related diseases.
Overweight is associated with worse health outcomes from COVID‑19, despite this, overweight risk factors increased during the pandemic
Policies to restrict movement during the COVID‑19 pandemic worsened overweight risk factors, in particular, levels of PA declined while sedentary behaviour increased. As a result, the proportion of people reporting weight gain during the pandemic was greater than those who reported weight loss.
OECD countries have responded to the obesity epidemic with a mixture of policy interventions
All OECD and EU27 countries have in place multiple national strategies to address key overweight risk factors including national dietary and physical activity guidelines. Strategies at the national level draw upon and complement action plans developed by the international community, such as WHO’s Global Action Plan on Physical Activity, which aims to reduce the global prevalence of physical inactivity by 15% by 2030.
Changing environmental factors that dictate lifestyle behaviours have fuelled overweight, which disproportionality affects poorer populations
While multiple factors contribute to a person’s weight, it is widely recognised that changes in body-mass index (BMI) are due to an imbalance between energy intake from diet and energy output through physical activity. For reasons discussed below, environments in which people live are increasingly considered “obesogenic” given they encourage people to eat more and move less (Swinburn, Egger and Raza, 1999[1]).
A multitude of factors has altered what and how much people eat. Advances in technology, globalisation, the expansion of food retail, rising incomes and urbanisation have changed the quantity and quality of calories consumed (Etilé and Oberlander, 2019[2]; Baker et al., 2020[3]). For example, today, mass-produced, ultra-processed foods (UPFs) are both cheap and readily accessible in countries across the world. As a result, among high-income countries, UPFs now make up “30‑60% of total dietary energy consumed”. Further, these aforementioned factors have contributed to the rise of “food swamps” characterised by areas with a high number of fast food outlets (OECD, 2021[4]).
Among OECD countries, the quantity of calories has increased, while the nutritional quality has worsened. Between 1961 and 2013, total food supply grew by 10% among OECD countries – or from 3 000 to 3 300 calories per capita, per day. EU27 countries recorded similar levels of growth (OECD, 2019[5]). Examining changes in calories alone is insufficient, given the quality of calories plays a key role in weight gain/loss. Today, consumption of nutrients associated with weight gain such as added fats and sugars, as well as saturated fat intake, primarily from animal sources, play a larger role in diets among OECD countries (WHO and FAO, 2003[6]). This comes at the expense of foods with healthy dietary elements such as fruit and vegetables and whole grain products, whose consumption is associated with weight loss. For example, over half of all adolescents do not consume fruit or vegetables each day (Figure 2.1), with similar figures recorded for adults. Further, UPFs, which are linked to higher calorie intake and worse health outcomes (Hall et al., 2019[7]) comprise over 50% of total energy intake in countries such as the United States and the United Kingdom (Marino et al., 2021[8]).
Figure 2.1. Share of 15‑year‑olds not consuming any fruit or vegetable each day, 2017‑18
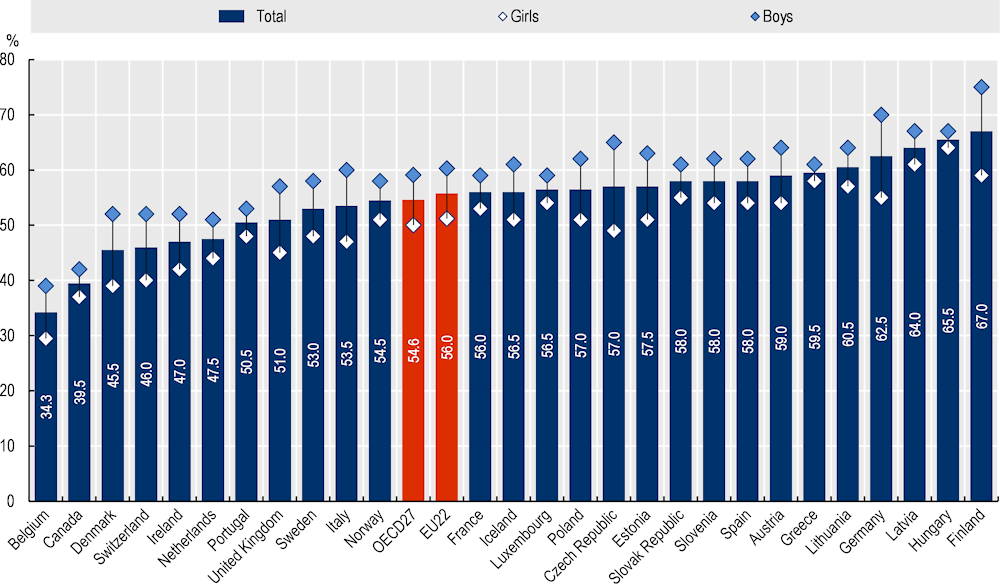
Source: Inchley et al. (2020[9]), “Spotlight on adolescent health and well-being. Findings from the 2017/2018 Health Behaviour in School-aged Children (HBSC) survey in Europe and Canada. International report. Volume 1. Key findings”, https://apps.who.int/iris/bitstream/handle/10665/332091/9789289055000-eng.pdf.
Physical activity is another key determinant of overweight.1 There are four areas where people are physically active throughout the day – at work or school, at home, during leisure time and when travelling (see Table 2.1). When combined, these four types of physical activity become the second largest contributor to total energy expenditure behind resting metabolic heart rate, (the rate at which your body burns energy when at complete rest) and before the thermic effect of feeding (energy used to digest and process food) (FAO, 2003[10]). Of the three contributors to energy expenditure, physical activity is the most modifiable and therefore a key policy area for promoting weight loss.
Table 2.1. Physical activity domains
|
Physical activity domain |
Example activities |
|---|---|
|
Leisure time |
Hobbies, sports and exercise |
|
Household |
Household chores such as gardening, shopping, child care, and incidental physical activity |
|
Occupation and schools |
Work-related physical activity (e.g. walking across a shop floor) |
|
Transportation |
Walking or cycling to work or public transport |
Source: Sallis et al. (2012[11]), “Role of Built Environments in Physical Activity, Obesity, and Cardiovascular Disease”, https://doi.org/10.1161/CIRCULATIONAHA.110.969022.
The benefits of physical activity extend beyond weight loss and management. Key benefits include an improvement in mental health, strengthening of bones, muscles and joints, as well as lowering the risk of illness (e.g. cardiovascular diseases, some commonly occurring cancers, Alzheimer’s disease, dementia, high blood pressure, and type 2 diabetes).
People today have fewer reasons to be physically active. Approximately a third of all adults in the OECD and EU are insufficiently active with figures ranging from just under 20% in Finland to up to 46% in Portugal. For all countries, levels of insufficient physical activity are higher for women than men (Figure 2.2). Low levels of physical activity reflect factors such as advances in technologies and changes to the built environment, which have given people fewer reasons to be physically active. For example, between 1990 and 2019, the number of passenger cars per 1 000 people – also known as the motorisation rate – grew by 88% among EU27 countries (Eurostat, 2019[12]). Further, as of 2019, cars are the predominant form of urban transport in the EU, which may in part reflect higher levels of car ownership (Eurostat, 2021[13]). Conversely, there is scientific consensus that people who live in “walkable” environments are more likely to have higher levels of physical activity (Mackett and Brown, 2011[14]). (Further details on physical activity trends and patterns are available in an upcoming joint OECD and WHO publication (forthcoming[15])).
Figure 2.2. Prevalence of insufficient physical activity
Prevalence of insufficient physical activity among adults aged 18+ years, crude estimate (%), 2016
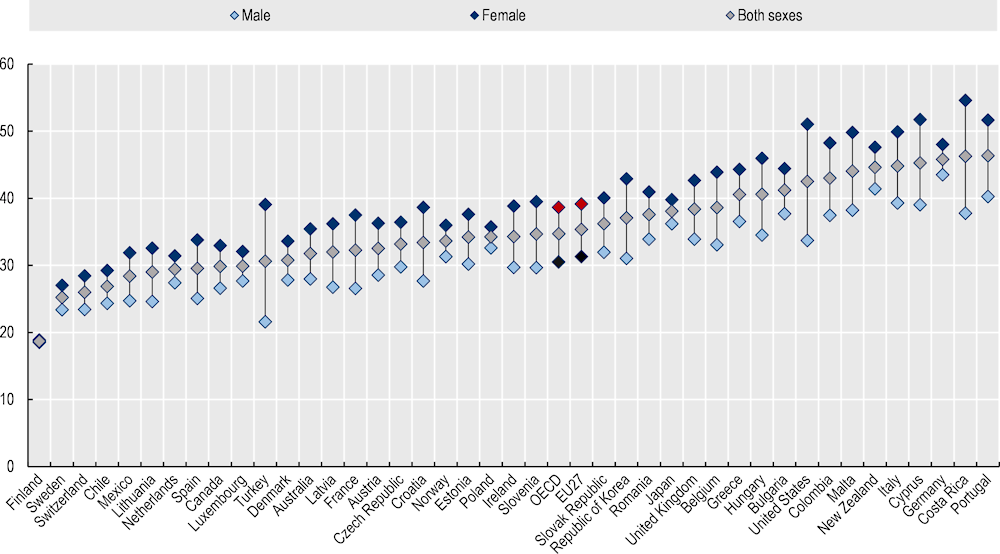
Source: WHO (2021[16]), “Prevalence of insufficient physical activity among adults aged 18+ years (crude estimate) (%)”, https://apps.who.int/gho/data/view.main.2463.
Levels of sedentary behaviour are also high. Similar to physical activity, sedentary behaviour is another key determinant of total energy expenditure and is therefore important to examine when discussing trends in overweight and obesity. Sedentary behaviour is defined as any behaviour when awake, which involves low energy expenditure (i.e. 1.5 metabolic equivalent of task (MET)2 or lower) such as sitting, reclining or in a lying posture (van der Ploeg and Hillsdon, 2017[17]). Levels of sedentary behaviour are high among OECD countries for a variety of reasons including the proliferation of labour-saving technologies, such as laptops (see Box 2.1). For example, nearly four in ten adults across the EU complete their work while sitting down, with figures as high as 54% in the Netherlands (Eurostat, 2017[18]). Further, in the United States, the average civilian worker sits for 43% of the workday (U.S. Bureau of Labor Statistics, 2020[19]). During the COVID‑19 pandemic, there is consensus among published papers that levels of sedentary behaviour worsened, for example due to an increase in daily screen time (OECD and WHO, forthcoming[15]).
Box 2.1. Sedentary behaviour is prevalent among OECD countries
A number of surveys have investigated levels of sedentary behaviour recorded across several OECD member countries:
Australia: the most recent data on levels of sedentary behaviour in Australia comes from the National Nutrition and Physical Activity Survey undertaken in 2011‑12. Results from this survey found just one in four children aged 2‑5 met sedentary screen-based behaviour guidelines, with this figure decreasing to one in five among those aged 13‑17 years (AIHW, 2018[20]).
EU: a Eurobarometer Survey undertaken in 2017 revealed 12% of the EU population spend over eight and a half hours a day sitting, ranging from 7% in Spain to 32% in the Netherlands (European Commission, 2017[21]).
Japan: a cross-sectional study covering nearly 2 000 Japanese adults aged 40 years and over found half of participant’s waking time was spent being sedentary, of which nearly a third was accumulated over long periods of time (i.e. >=30 minutes) (Chen et al., 2018[22]).
United States: a cross-sectional study in the United States covering 50 000 children aged five years and over found 62% of children spent at least two hours a day sitting watching television or videos with this figure increasing to 65% among adults (Yang et al., 2019[23]).
There is growing recognition that changes to the food and physical environment are not solely responsible for rising rates of overweight. Other modifiable risk factors that contribute to a person’s weight gain/loss include stress levels, sleep and the gut microbiota:
Sleep: sleep deprivation can affect a person’s energy intake/output through several channels including increasing hunger, allowing people more time to eat and decreasing levels of physical activity due to fatigue. Several studies are now available measuring the link between sleep and weight in both children and adults. Among young people, a meta‑analysis suggest there is an association between poor sleep quality and overweight and obesity (e.g. young adults who experience inadequate sleep are 27% more likely to live with overweight) (Fatima, Doi and Mamun, 2016[24]). Similarly for adults, a recent systematic review and meta‑analysis concluded there is a significant association between short sleep duration and risk of future obesity (Bacaro et al., 2020[25]).
Stress: stress due to work, personal or financial strain can negatively impact a person’s energy intake/output leading to weight gain, for example, due to “euroendocrine and inflammatory pathways that directly increase abdominal adiposity” as well as a preference for high energy foods (Harding et al., 2013[26]). A longitudinal study of over 5 000 Australian adults found those with perceived high levels of stress experienced a 0.20kg/m2 greater gain in BMI compared to those with low stress levels (Harding et al., 2013[26]).
Gut microbiota: microbiota plays a key function within the human body, for example, by regulating the immune system, food digestion and production of key vitamins. A diverse gut microbiota consisting of different types of microorganisms (e.g. bacteria and fungi) is considered healthy and is largely influenced by a person’s diet. For example, there is emerging evidence indicating an association between a gut microbiota with reduced diversity3 and obesity (Kim et al., 2020[27]). People can create more diverse gut microbiota by consuming a diet rich in a variety of fruits, vegetables, legumes, nuts, seeds and whole grains. Further, there is evidence to show that a plant-based diet is also good for the environment (see Box 2.2).
Box 2.2. Diets and climate change
Changes in human activities including the burning of fossil fuels, deforestation and farming of livestock have drastically increased the level of greenhouse gas emissions emitted into the atmosphere. Consequently, the global temperature has risen rapidly and without action will continue to increase leading to more extreme weather events and rising sea levels.
One way to reduce levels of greenhouse gas emissions is to change what people eat. Specifically, away from meats and towards a more plant-based diet (The EAT-Lancet Commission, 2022[28]). This is because meat, in particular red meats, has a markedly higher carbon footprint when compared to plant-based foods due to land use, methane emissions and crop production to feed animals. For example, beef emits 60kg CO2‑equivalents per kilogram compared to 6kg for poultry meat and 1.4kg for wheat and rye (Poore and Nemecek, 2018[29]).
Rates of overweight and obesity for both adults and adolescents have been rising and are higher for men. Between 1996 and 2016, the proportion of men and women in the OECD living with obesity increased by 10 and 7 percentage points, respectively (WHO, 2016[30]). Consequently, as of 2016, nearly one in four adults in the OECD live with obesity. Over the same period (1996‑2016), the proportion of children aged between five and nine considered overweight increased from 21% to 31% (OECD, 2019[31]). More recent estimates (2019) from a smaller number of countries that report measured data suggest rates of overweight, which includes obesity, are even higher at around 64% and 56% of men and women in the OECD, respectively (see Figure 2.3).
Figure 2.3. Measured overweight (including obesity) rates among adults, 2019 (or nearest year)
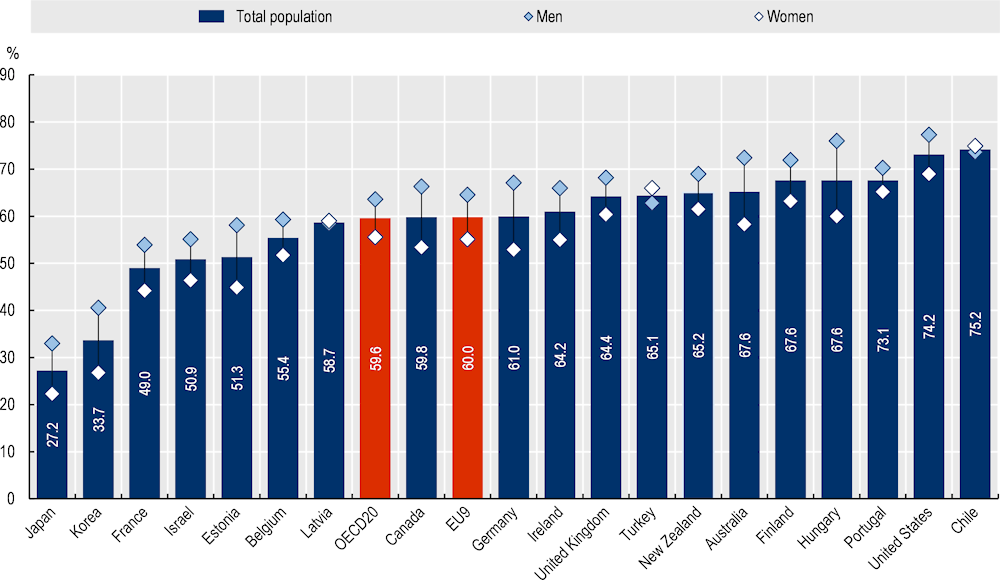
Note: The OECD average is unweighted.
Source: OECD Health Statistics 2021, https://doi.org/10.1787/health-data-en.
Overweight is more prevalent among lower socio‑economic groups. As previously discussed, people increasingly live in obesogenic environments. Individuals with a higher socio‑economic status (SES) are better equipped to live in such an environment – for example, higher educated individuals may have a better understanding of what constitutes a healthy lifestyle and the resources to pursue this way of life (Devaux et al., 2011[32]; Placzek, 2021[33]). Data from the Health Behaviour in School-aged Children (HBSC) survey 2017/18 reflect this theory with 26% of 15‑year‑olds with a low family affluence status (FAS) report being overweight compared to 16% among those with a high FAS (Figure 2.4) (Inchley et al., 2020[9]).
Figure 2.4. Self-reported overweight (including obese) in 15‑year‑olds, by family affluence, 2017‑18
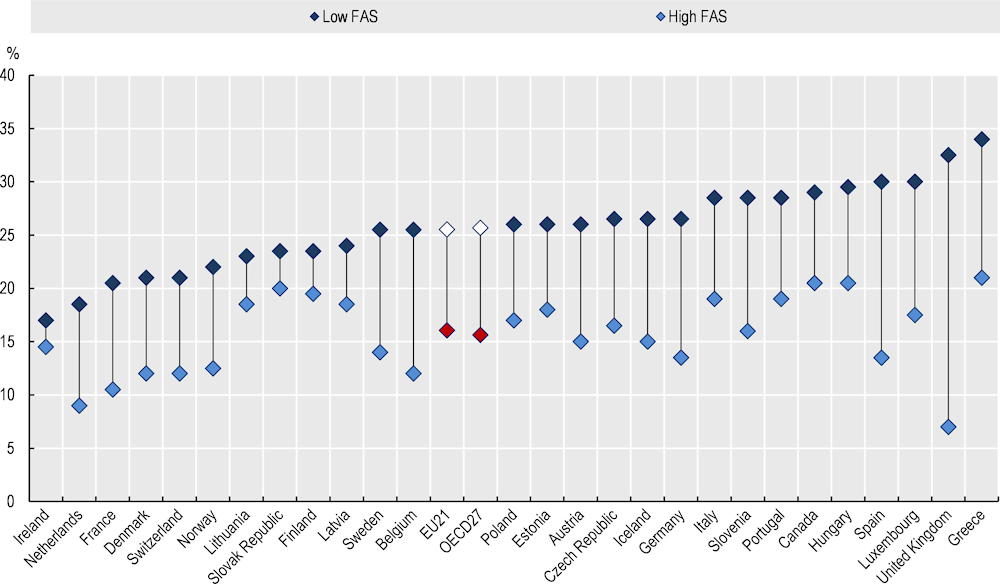
Note: FAS = Family affluence status.
Source: Inchley et al. (2020[9]), “Spotlight on adolescent health and well-being. Findings from the 2017/2018 Health Behaviour in School-aged Children (HBSC) survey in Europe and Canada. International report. Volume 1. Key findings”, https://apps.who.int/iris/bitstream/handle/10665/332091/9789289055000-eng.pdf.
Overweight has a heavy toll on both health and economic outcomes
Overweight in adults worsens health outcomes and shortens life expectancy. Adults who live with overweight are at greater risk of developing non-communicable diseases (NCDs) including type 2 diabetes, several cancers, stroke, and asthma (Nyberg et al., 2018[34]). Modelling work undertaken by OECD across 52 countries4 estimates that between years 2020 and 2050, overweight and obesity will cause an additional 462 million cases of cardiovascular disease (CVD) and 212 million new cases of diabetes. Respectively, these figures represent 18% and 58% of all new cases (OECD, 2019[5]). In turn, higher incidence of NCDs causes premature mortality and therefore a decline in overall life expectancy (LE): over the same period (2020‑50), overweight and obesity is estimated to reduce average LE in the OECD by 2.7 years, with this figure increasing to 3.2 years when considering healthy life years (HALE) (OECD, 2019[5]) (Figure 2.5).
Figure 2.5. The impact of overweight and obesity on life expectancy and healthy life expectancy in years, average for 2020‑50
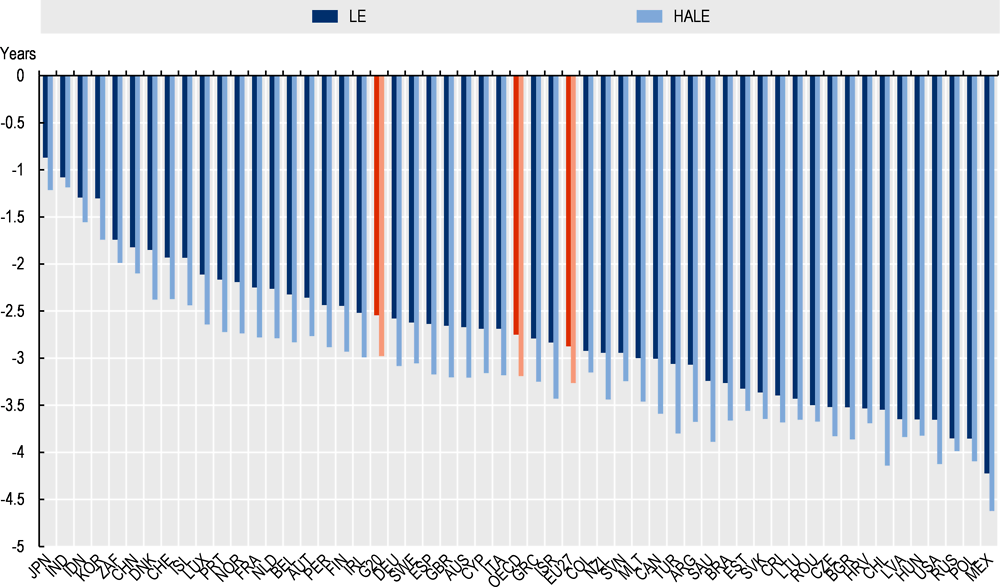
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2019.
Negative health effects associated with excessive weight also occur during early years of life. Overweight in childhood is a key determinant of obesity in adulthood, which, as previously mentioned, is associated with a range of NCDs. Children living with overweight may also experience health issues at an early age including breathing difficulties, insulin resistance and hypertension. Overweight at a young age can also cause higher levels of mental distress, for example, due to bullying: OECD analysis found boys aged 11‑15 living with obesity are nearly twice as likely to be bullied when compared to their normal weight peers, with this figure increasing to three times as likely for girls (OECD, 2019[5]).
Overweight has a direct impact on health expenditure by increasing demand for health care services. People with overweight are more likely to develop one or multiple NCDs. Consequently demand for health care services that treat and manage NCDs rises. Not only does overweight increase the frequency of contact with the health care system, it also increases the cost per contact as treatment is often more complex (Bertakis and Azari, 2005[35]). OECD analysis estimates that treating overweight and its related conditions cost countries, on average, an additional USD PPP (purchasing power parity) 209 annually per capita, which translates into 8.4% of total health expenditure (Figure 2.6).
Figure 2.6. Estimated health expenditure associated with overweight
Health expenditure due to overweight per year, in USD PPP per capita and as a percentage of total health expenditure, average 2020‑50
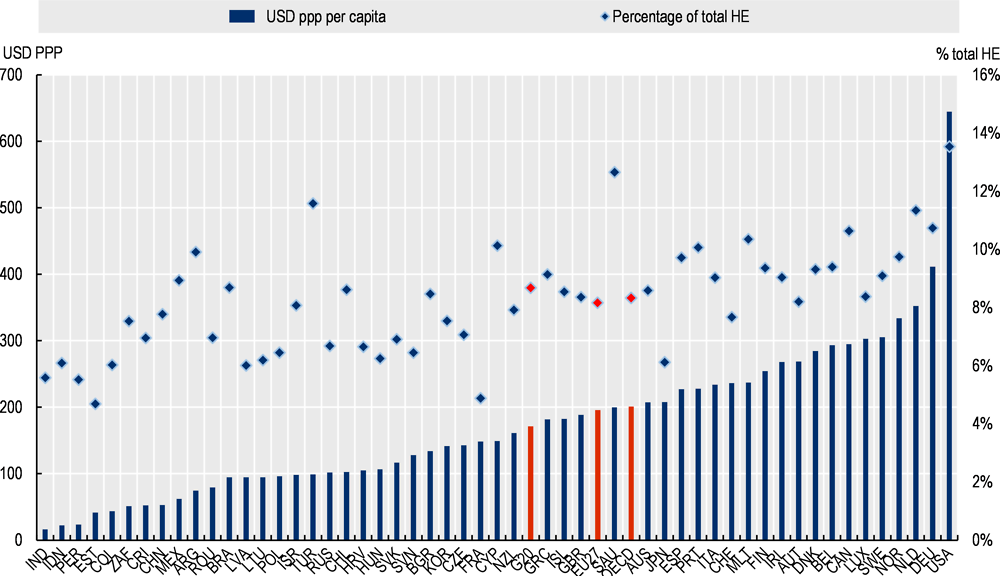
Source: OECD analyses based on the OECD SPHeP-NCDs model, 2019.
Overweight has an indirect negative impact on economic outcomes by depressing workforce productivity. Overweight and its related health issues reduce productivity among working-age adults, for example, through absenteeism and early retirement. Across OECD countries, overweight is estimated to reduce workforce productivity, on average, by ‑1.66% per capita, per year. When combining the impact on the workforce and life expectancy, overweight is estimated to reduce GDP by 3.3% per year on average across OECD countries.
Overweight is associated with worse health outcomes from COVID‑19, despite this, overweight risk factors increased during the pandemic
People living with overweight, and obesity in particular, are at greater risk of developing severe symptoms and dying from COVID‑19. For example, a study by Tartof et al. (2020[36]) using data from a United States integrated health care organisation, found compared to patients with a “normal weight” (BMI between 18.5‑24 kg/m2), morbidly obese patients are between 2.68 (BMI 40‑44 kg/m2) and 4.18 (BMI > 45 kg/m2) times more likely to die from COVID‑19. Similarly, several studies show that obesity increases the risk of developing severe COVID‑19 symptoms as measured by hospitalisations, including intensive care unit admissions (CDC, n.d.[37]; Public Health England, 2020[38]; Yang, Hu and Zhu, 2020[39]; the LICORN and the Lille COVID‐19 and Obesity study group, 2020[40]; Popkin et al., 2020[41]; World Obesity Federation, 2021[42]).
The COVID‑19 pandemic had a negative impact on lifestyle behaviours resulting in weight gain. OECD countries responded to the COVID‑19 pandemic by introducing “lockdowns” as a way to reduce disease transmission. This significantly altered people’s daily lives including how they eat and exercise. It is too soon to conclude what long-term impact the pandemic had on peoples weight, however, studies on short-term weight gain/loss as well as overweight risk factors are available. For example, results from an Ipsos survey covering 19 OECD countries found that in all countries, the proportion of the population who reported gaining weight during the pandemic was greater than those reporting losing weight (Figure 2.7) (Bailey et al., 2021[43]). A summary of studies looking at the impact of COVID‑19 on overweight risk factors is available in Box 2.3.
Figure 2.7. Proportion of the population reporting weight gain/loss during the COVID‑19 pandemic
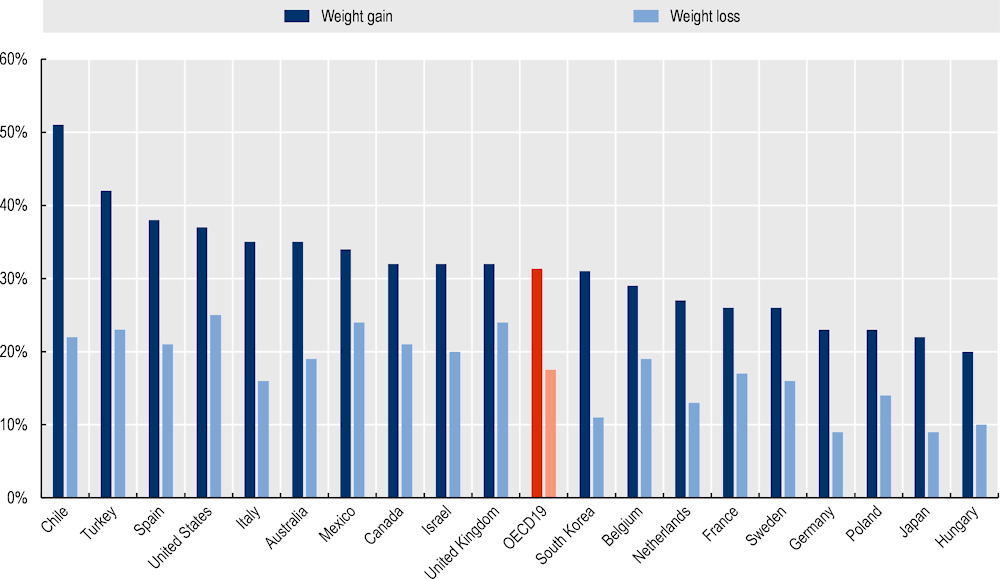
Source: Bailey et al. (2021[43]), “Diet & Health under COVID‑19”, https://www.ipsos.com/sites/default/files/ct/news/documents/2021-01/diet-and-health-under-covid-19.pdf.
Box 2.3. The impact of COVID‑19 on overweight risk factors
Provided below is summary of key findings from studies analysing the impact of the COVID‑19 pandemic on eating habits and physical activity:
A survey by Bailey et al. (2021[43]) found that, on average, 22% of people living in OECD19 countries increased the amount they exercised compared to 25% who decreased the amount they exercised.
Stockwell et al. (2021[44]) undertook a systematic review to understand the impact of the pandemic on physical activity and sedentary behaviour. The review included 66 studies covering nearly 90 000 people aged between 13 and 86 years. The majority of studies included in the review found a decline in physical activity and an increase in sedentary behaviour despite guidance on how to stay active in lockdown.
Stavridou et al. (2021[45]) focused their literature review on the impact of the pandemic on overweight among children and adolescents. Their review, which covered nearly 40 000 subjects, found an increase in the number of meals eaten as well as intake of potatoes, meat and sugary drinks. Further, due to a restriction in movement, levels of physical activity declined while sedentary behaviour increased.
Findings from a multinational survey covering 14 countries (10 of which were OECD members) found self-reported levels of moderate‑vigorous physical activity as well as vigorous physical activity declined during COVID‑19 restrictions. No significant differences were found between men and women, however, those with high levels of physical activity prior to the pandemic reported greater decreases than those who were less active (Wilke et al., 2021[46]).
OECD countries have responded to the obesity epidemic with a mixture of policy interventions
Overweight is a top political priority in the OECD given its detrimental impact on health and economic outcomes. Overweight causes health expenditure to rise and productivity in the workforce to lower. Given the wide‑reaching impact of overweight, governments in the OECD have responded by developing overarching national action plans addressing the determinants of overweight. These include, but are not limited to, policies to guide national dietary and physical activity guidelines, as well as adult and childhood overweight specific strategies. As shown in Figure 2.8, all OECD and EU27 countries have in place multiple national strategies to address high rates of overweight. The data in Figure 2.8 is supported by more recent information collected by WHO which found that, as of 2019, 92% of OECD and 89% of EU27 countries have a national action plan for unhealthy diets and physical inactivity (WHO, 2019[47]; WHO, 2019[48]). A few examples of strategies to tackle the determinants of obesity at the country level are listed below:
United States:
Active People, Healthy NationSM is led by the Centers for Disease Control and Prevention (CDC) to encourage young people and adults to be more active by 2027
Healthy People 2030 sets out data-driven objectives to improve overall health and well-being, including a reduction in the proportion of children, adolescents and adults living with obesity.
Australia:
The National Preventive Health Strategy 2021‑30 (further details are available in Box 1.2).
Figure 2.8. National action plans to address overweight and obesity – OECD and EU27 countries
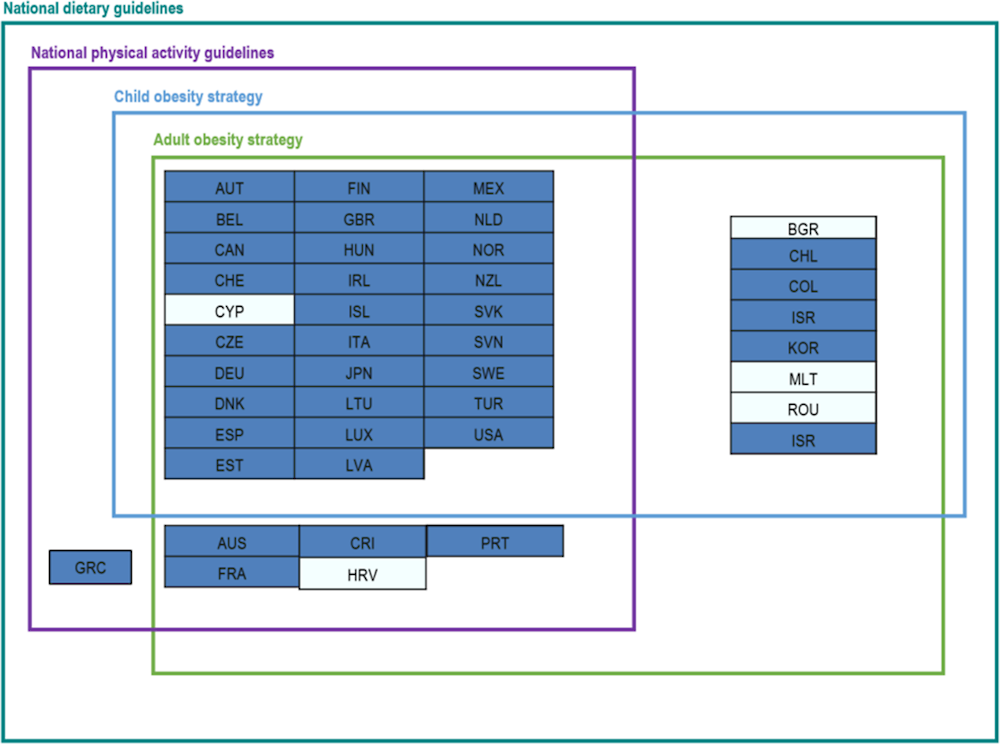
Note: OECD countries are in dark blue and non-OECD EU27 countries in light blue.
Source: WCRFI (2016[49]), “Nourishing framework”, http://www.wcrf.org/int/policy/nourishing-framework; Development Initiatives (2018[50]), “2018 Global Nutrition Report: Shining a light to spur action on nutrition”, https://globalnutritionreport.org/d7447a; WHO (2012[51]), “Global database on the Implementation of Nutrition Action (GINA)”, https://www.who.int/nutrition/gina/en/; WHO Regional Office for Europe (2021[52]), “2021 Physical Activity Factsheets for the European Union Member States in the WHO European Region”, https://apps.who.int/iris/bitstream/handle/10665/345335/WHO-EURO-2021-3409-43168-60449-eng.pdf.
Plans at the national level align with international policies to tackle overweight. Overweight is global issue affecting both developing and developed countries. In response, the international community has responded by developing overarching goals and strategies to address this growing public health issue. Prominent examples include:
The United Nation’s (UN) Sustainable Development Goals, which has a target to reduce premature mortality from NCDs by one‑third through prevention and treatment by 2030
WHO’s Global Action Plan on Physical Activity, which aims to reduce the global prevalence of physical inactivity by 15%, also by 2030
WHO’s Physical Activity Strategy for the WHO European Region 2016‑25, which provides a blueprint to incentivise Member States to act (WHO, 2013[53]; Breda et al., 2018[54])
Europe’s Beating Cancer Plan recognises that obesity is a key risk factor for cancer and therefore must be addressed (European Commission, 2021[55])
The EU’s Farm to Fork Strategy, which among other things, aims to ensure people have access to nutritious foods (European Commission, 2019[56])
The two‑year campaign, HealthyLifestyle4All (EC, 2021[57]), which is a follow-up of the Tartu Call for a Healthy Lifestyle, was launched in September 2021 to showcase the European Commission’s continuous commitment to promoting a healthy lifestyle across generations and social groups.
Comprehensive policy packages that draw upon international best practice are necessary to tackle the determinants of overweight. Overweight is a complex issue that affects people from all different backgrounds and ages. For this reason, no single policy can tackle this health issue, rather, a suite of complementary policies that create an environment supportive of healthy eating and physical activity is needed. At a high-level, OECD has grouped policies to tackle overweight into four broad domains (Figure 2.9). These domains align with frameworks and policy advice from the WHO, including “Best Buy” interventions for preventing and controlling NCDs, as well as the Global Action Plan on Physical Activity (2018‑30) (WHO, 2018[58]).
Figure 2.9. OECD’s policy framework for tackling overweight

Source: Taken from OECD (2019[5]), The Heavy Burden of Obesity: The Economics of Prevention, https://dx.doi.org/10.1787/67450d67-en.
Subsequent chapters to this report analyse 12 interventions targeting overweight risk factors – i.e. unhealthy diets and/or physical inactivity. Table 2.2 lists each analysed intervention accompanied by a high-level description. The vast majority of interventions analysed in this report reflect policies that aim to influence people’s choices (see Figure 2.9) – for example, by providing education on how to eat more nutritious foods and be more active, as well as labelling foods to highlight those associated with a healthy diet and weight loss.
Table 2.2. Case study interventions
|
Intervention |
Description |
Type of obesity policy |
|---|---|---|
|
Nutri-Score |
Front-of-pack labelling intervention to address unhealthy eating |
Influencing choices |
|
Physical Activity on Prescription (PAP) |
Intervention to prescribe patients physical activity in a primary care setting |
Influencing choices |
|
Combined Lifestyle Intervention (CLI) |
Primary care intervention offered to those who are overweight or obese. Patients are guided on how to improve diet, exercise and overall health. |
Influencing choices |
|
Multimodal Training Intervention (MTI) |
Physical activity and healthy eating programme targeting those aged 65 years and older. |
Influencing and widening choices |
|
Young People at a Healthy Weight (JOGG) |
Community-based intervention designed to improve diets and boost physical activity among those aged 0‑19 years |
Influencing and widening choices |
|
ToyBox |
Kindergarten intervention to improve healthy eating and physical activity |
Influencing choices |
|
Danish Whole Grain Partnership |
A front-of-pack labelling intervention to boost wholegrain consumption |
Influencing choices |
|
StopDia Pilot for the Somali population |
Lifestyle intervention for the Somali population who are at-risk of developing type 2 diabetes (adapted from the nation-wide StopDia intervention) |
Influencing choices |
|
SI! intervention |
Multidimensional school-based obesity prevention intervention, which targets lifestyle behaviour changes in 3‑5 year‑olds |
Influencing choices |
|
Diabetes in Europe – Prevention using Lifestyle, Physical Activity and Nutrition (DE‑PLAN) |
Type 2 diabetes prevention intervention aimed at improving diet and physical activity levels through a lifestyle, community-based intervention |
Influencing choices |
|
Personalised Approach to Obesity Management in Children (PAOMC) |
Clinical, family-based and personalised childhood obesity programme targeting children aged 7 to 17 years |
Influencing choices |
|
Let Food Be Your Medicine |
Personalised nutrition mHealth app |
Influencing choices |
References
[20] AIHW (2018), Physical activity across the life stages, https://www.aihw.gov.au/reports/physical-activity/physical-activity-across-the-life-stages/contents/table-of-contents.
[25] Bacaro, V. et al. (2020), “Sleep duration and obesity in adulthood: An updated systematic review and meta-analysis”, Obesity Research & Clinical Practice, Vol. 14/4, pp. 301-309, https://doi.org/10.1016/j.orcp.2020.03.004.
[43] Bailey, P. et al. (2021), Diet & Health under COVID-19, Ipsos, https://www.ipsos.com/sites/default/files/ct/news/documents/2021-01/diet-and-health-under-covid-19.pdf (accessed on 3 May 2021).
[3] Baker, P. et al. (2020), “Ultra‐processed foods and the nutrition transition: Global, regional and national trends, food systems transformations and political economy drivers”, Obesity Reviews, Vol. 21/12, https://doi.org/10.1111/obr.13126.
[35] Bertakis, K. and R. Azari (2005), “Obesity and the Use of Health Care Services”, Obesity Research, Vol. 13/2, pp. 372-379, https://doi.org/10.1038/oby.2005.49.
[54] Breda, J. et al. (2018), “Promoting health-enhancing physical activity in Europe: Current state of surveillance, policy development and implementation”, Health Policy, Vol. 122/5, pp. 519-527, https://doi.org/10.1016/j.healthpol.2018.01.015.
[37] CDC (n.d.), Obesity, Race/Ethnicity, and COVID-19 | Overweight & Obesity, https://www.cdc.gov/obesity/data/obesity-and-covid-19.html.
[22] Chen, T. et al. (2018), “Patterns and Levels of Sedentary Behavior and Physical Activity in a General Japanese Population: The Hisayama Study”, Journal of Epidemiology, Vol. 28/5, pp. 260-265, https://doi.org/10.2188/jea.je20170012.
[32] Devaux, M. et al. (2011), “Exploring the Relationship Between Education and Obesity”, OECD Journal: Economic Studies, https://doi.org/10.1787/eco_studies-2011-5kg5825v1k23.
[50] Development Initiatives (2018), 2018 Global Nutrition Report: Shining a light to spur action on nutrition, Development Initiatives, https://globalnutritionreport.org/d7447a.
[57] EC (2021), The HealthyLifestyle4All Initiative, https://sport.ec.europa.eu/initiatives/healthylifestyle4all (accessed on 20 October 2021).
[2] Etilé, F. and L. Oberlander (2019), The Economics of Diet and Obesity: Understanding the Global Trends, Oxford University Press, https://doi.org/10.1093/acrefore/9780190625979.013.19.
[55] European Commission (2021), Europe’s Beating Cancer Plan, https://ec.europa.eu/health/sites/default/files/non_communicable_diseases/docs/eu_cancer-plan_en.pdf.
[56] European Commission (2019), Farm to Fork Strategy: For a fair, healthy and environmentally-friendly food system, https://ec.europa.eu/food/sites/food/files/safety/docs/f2f_action-plan_2020_strategy-info_en.pdf.
[21] European Commission (2017), Special Eurobarometer 472: Sport and physical activity, https://data.europa.eu/data/datasets/s2164_88_4_472_eng?locale=en.
[13] Eurostat (2021), Passenger mobility statistics, https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Passenger_mobility_statistics#Travel_mode.
[12] Eurostat (2019), Passenger cars per 1 000 inhabitants.
[18] Eurostat (2017), Persons performing physical activity when working by type of activity, most frequent activity status, quantile and degree of urbanization.
[10] FAO (2003), Human energy requirements: Principles and definitions, https://www.fao.org/3/y5686e/y5686e04.htm.
[24] Fatima, Y., S. Doi and A. Mamun (2016), “Sleep quality and obesity in young subjects: a meta-analysis”, Obesity Reviews, Vol. 17/11, pp. 1154-1166, https://doi.org/10.1111/obr.12444.
[7] Hall, K. et al. (2019), “Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake”, Cell Metabolism, Vol. 30/1, pp. 67-77.e3, https://doi.org/10.1016/j.cmet.2019.05.008.
[26] Harding, J. et al. (2013), “Psychosocial stress is positively associated with body mass index gain over 5 years: Evidence from the longitudinal AusDiab study”, Obesity, Vol. 22/1, pp. 277-286, https://doi.org/10.1002/oby.20423.
[9] Inchley, J. et al. (2020), Spotlight on adolescent health and well-being. Findings from the 2017/2018 Health Behaviour in School-aged Children (HBSC) survey in Europe and Canada. International report. Volume 1. Key findings, https://apps.who.int/iris/bitstream/handle/10665/332091/9789289055000-eng.pdf.
[27] Kim, M. et al. (2020), “Gut microbiota and metabolic health among overweight and obese individuals”, Scientific Reports, Vol. 10/1, https://doi.org/10.1038/s41598-020-76474-8.
[14] Mackett, R. and B. Brown (2011), Transport, Physical Activity and Health: Present knowledge and the way ahead, UCL, http://www.cege.ucl.ac.uk/research/projects?sq_content_src=%2BdXJsPWh0dHAlM0ElMkYlMkZ3d3cyLmNlZ2UudWNsLmFjLnVrJTJGcmVzZWFyY2glMkZSZXNQcm9qRGV0LmFzcCUzRklEJTNEMTc0JmFsbD0x (accessed on 25 October 2021).
[8] Marino, M. et al. (2021), “A Systematic Review of Worldwide Consumption of Ultra-Processed Foods: Findings and Criticisms”, Nutrients, Vol. 13/8, p. 2778, https://doi.org/10.3390/nu13082778.
[34] Nyberg, S. et al. (2018), “Obesity and loss of disease-free years owing to major non-communicable diseases: a multicohort study”, The Lancet Public Health, Vol. 3/10, pp. e490-e497, https://doi.org/10.1016/s2468-2667(18)30139-7.
[4] OECD (2021), Making Better Policies for Food Systems, OECD Publishing, Paris, https://doi.org/10.1787/ddfba4de-en.
[31] OECD (2019), Health at a Glance 2019: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/4dd50c09-en.
[5] OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/67450d67-en.
[15] OECD and WHO (forthcoming), The Burden of Physical Inactivity, OECD Publishing, Paris.
[33] Placzek, O. (2021), “Socio-economic and demographic aspects of food security and nutrition”, OECD Food, Agriculture and Fisheries Papers, No. 150, OECD Publishing, Paris, https://doi.org/10.1787/49d7059f-en.
[29] Poore, J. and T. Nemecek (2018), “Reducing food’s environmental impacts through producers and consumers”, Science, Vol. 360/6392, pp. 987-992, https://doi.org/10.1126/science.aaq0216.
[41] Popkin, B. et al. (2020), “Individuals with obesity and COVID‐19: A global perspective on the epidemiology and biological relationships”, Obesity Reviews, Vol. 21/11, https://doi.org/10.1111/obr.13128.
[38] Public Health England (2020), Excess Weight and COVID-19: Insights from new evidence, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/907966/PHE_insight_Excess_weight_and_COVID-19__FINAL.pdf.
[11] Sallis, J. et al. (2012), “Role of Built Environments in Physical Activity, Obesity, and Cardiovascular Disease”, Circulation, Vol. 125/5, pp. 729-737, https://doi.org/10.1161/circulationaha.110.969022.
[45] Stavridou, A. et al. (2021), “Obesity in Children and Adolescents during COVID-19 Pandemic”, Children, Vol. 8/2, p. 135, https://doi.org/10.3390/children8020135.
[44] Stockwell, S. et al. (2021), “Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review”, BMJ Open Sport & Exercise Medicine, Vol. 7/1, p. e000960, https://doi.org/10.1136/bmjsem-2020-000960.
[1] Swinburn, B., G. Egger and F. Raza (1999), “Dissecting Obesogenic Environments: The Development and Application of a Framework for Identifying and Prioritizing Environmental Interventions for Obesity”, Preventive Medicine, Vol. 29/6, pp. 563-570, https://doi.org/10.1006/pmed.1999.0585.
[36] Tartof, S. et al. (2020), “Obesity and Mortality Among Patients Diagnosed With COVID-19: Results From an Integrated Health Care Organization”, Annals of Internal Medicine, Vol. 173/10, pp. 773-781, https://doi.org/10.7326/m20-3742.
[28] The EAT-Lancet Commission (2022), The Planetary Health Diet, https://eatforum.org/eat-lancet-commission/the-planetary-health-diet-and-you/.
[40] the LICORN and the Lille COVID‐19 and Obesity study group (2020), “High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus‐2 (SARS‐CoV‐2) Requiring Invasive Mechanical Ventilation”, Obesity, Vol. 28/7, pp. 1195-1199, https://doi.org/10.1002/oby.22831.
[19] U.S. Bureau of Labor Statistics (2020), Occupational Requirements Survey: Sitting and standing, https://www.bls.gov/ors/factsheet/sit-and-stand.htm.
[60] Valdes, A. et al. (2018), “Role of the gut microbiota in nutrition and health”, BMJ, p. k2179, https://doi.org/10.1136/bmj.k2179.
[17] van der Ploeg, H. and M. Hillsdon (2017), “Is sedentary behaviour just physical inactivity by another name?”, International Journal of Behavioral Nutrition and Physical Activity, Vol. 14/1, https://doi.org/10.1186/s12966-017-0601-0.
[49] WCRFI (2016), NOURISHING-framework, https://www.wcrf.org/policy/policy-databases/nourishing-framework/.
[16] WHO (2021), Prevalence of insufficient physical activity among adults aged 18+ years (crude estimate) (%).
[59] WHO (2019), Body mass index - BMI, https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi.
[47] WHO (2019), “Existence of operational policy/strategy/action plan to reduce physical inactivity”.
[48] WHO (2019), Existence of operational policy/strategy/action plan to reduce unhealthy diet related to NCDs (Noncommunicable diseases), https://apps.who.int/gho/data/node.imr.NCD_CCS_DietPlan?lang=en.
[58] WHO (2018), Global Action Plan On Physical Activity 2018-2030: More Active People For A Healthier World-2030, WHO, Geneva, http://apps.who.int/iris/bitstream/handle/10665/272722/9789241514187-eng.pdf?ua=1 (accessed on 3 June 2021).
[30] WHO (2016), Prevalence of obesity among adults, BMI & GreaterEqual; 30 (age-standardized estimate) (%), https://apps.who.int/gho/data/view.main.CTRY2450A.
[53] WHO (2013), Physical activity strategy for the WHO European Region 2016–2025, https://www.euro.who.int/en/publications/abstracts/physical-activity-strategy-for-the-who-european-region-20162025 (accessed on 20 October 2021).
[51] WHO (2012), Global database on the Implementation of Nutrition Action (GINA), https://www.who.int/nutrition/gina/en/.
[52] WHO Regional Office for Europe (2021), 2021 Physical Activity Factsheets for the European Union Member States in the WHO European Region, https://apps.who.int/iris/bitstream/handle/10665/345335/WHO-EURO-2021-3409-43168-60449-eng.pdf.
[6] WHO and FAO (2003), Diet, nutrition and the prevention of chronic diseases, WHO Technical Report Series 916, https://www.fao.org/3/ac911e/ac911e00.pdf.
[46] Wilke, J. et al. (2021), “A Pandemic within the Pandemic? Physical Activity Levels Substantially Decreased in Countries Affected by COVID-19”, International Journal of Environmental Research and Public Health, Vol. 18/5, p. 2235, https://doi.org/10.3390/ijerph18052235.
[42] World Obesity Federation (2021), COVID-19 and Obesity: The 2021 Atlas, https://www.worldobesityday.org/assets/downloads/COVID-19_and_Obesity-The_2021_Atlas.pdf.
[39] Yang, J., J. Hu and C. Zhu (2020), “Obesity aggravates COVID‐19: A systematic review and meta‐analysis”, Journal of Medical Virology, Vol. 93/1, pp. 257-261, https://doi.org/10.1002/jmv.26237.
[23] Yang, L. et al. (2019), “Trends in Sedentary Behavior Among the US Population, 2001-2016”, JAMA, Vol. 321/16, p. 1587, https://doi.org/10.1001/jama.2019.3636.
Notes
← 1. For adults, WHO define overweight and obesity as having a BMI >=25Kg/m2 and 30Kg/m2, respectively. BMI is the most widely used proxy for body adiposity to assess population-level rates of overweight, as it is easily derived from a person’s weight and height (i.e. weight (kg) divided by height in metres squared) (WHO, 2019[59]).
← 2. Metabolic equivalent of task (MET) is a measure to reflect the intensity of physical activities, and allows comparison between them. One MET is the energy equivalent expended per unit of time by an individual while seated at rest. More intense activities, which cost more energy expenditure than being seated at rest, are attributed higher METs.
← 3. Microbiota diversity “a measure of how many different species and, dependent on the diversity indices, how evenly distributed they are in the community. Lower diversity is considered a marker of dysbiosis (microbial imbalance) in the gut and has been found in autoimmune diseases and obesity and cardiometabolic conditions, as well as in elderly people” (Valdes et al., 2018[60]).
← 4. Includes all OECD countries, non-OECD European countries, non-OECD G20 countries as well as OECD accession and partner countries.