This chapter covers the Badalona Healthcare Service (BSA), an integrated care organisation. The case study includes an assessment of BSA against the five best practice criteria, policy options to enhance performance and an assessment of its transferability to other OECD and EU27 countries.
Integrating Care to Prevent and Manage Chronic Diseases

7. Badalona Healthcare Services (Badalona Serveis Assistencials, BSA), Spain
Abstract
BSA, an integrated care organisation: Case study overview
Description: In 2000, the Badalona City Council developed an integrated care organisation bringing together health and social care sectors – Badalona Serveis Assistencials, BSA. In addition to organisational integration (i.e. combining and health and social care), BSA creates other form of integration such as professional integration with the use of multidisciplinary teams and normative integration by developing a shared organisational and professional culture.
Best practice assessment:
OECD best practice assessment of BSA, an integrated care organisation
|
Criteria |
Assessment |
|---|---|
|
Effectiveness |
|
|
Efficiency |
|
|
Equity |
|
|
Evidence‑base |
|
|
Extent of coverage |
|
Enhancement options: To enhance effectiveness it is important that all health and social care providers have the skills and confidence to deliver multidisciplinary care, and are supportive of this new model of care. To enhance equity, BSA administrators could consider developing permanent programs dedicated to needs of disadvantaged groups with worse health profiles. To enhance the evidence‑base, future research should focus on evaluating the effectiveness and efficiency of BSA as a whole as opposed to individual programs within the integrated care organisation.
Transferability: The BSA integrated care organisation has not explicitly been transferred to other countries. In general, this model of care is more transferable to countries with a national health system (as opposed to insurance‑based models), a sophisticated health information system and a workforce supportive of multidisciplinary work.
Conclusion: BSA is an integrated care organisation bringing together health and social care services, and is supported by a sophisticated health information system. Programs within BSA have demonstrated an overall positive impact, however, the impact of BSA as a whole is unknown. Despite aligning with best practice, there are several options available to policy makers to enhance the performance of BSA.
Intervention description
Spain, like many OECD countries, has experienced a rise in the rate of people living with complex health needs. As of 2020, over a third of adults in Spain (37%) report living with a long-standing illness or health problem. Not only is this one of the highest rates in the EU, it is also markedly higher than the rate reported in 2011 (i.e. 21%) (Eurostat, 2022[1]). Rising numbers of people living with complex health needs stems from ageing population partnered with poor lifestyle habits, for example, unhealthy diets and limited physical activity.
New models of care have emerged to improve treatment for patients with complex health needs. Patients with complex health needs often require care from several health professionals working at different levels of care. For this reason, policy makers, including those in Spain, have implemented new models of care which offer integrated, co‑ordinated care centred around patient needs (Monterde et al., 2020[2]; Dueñas-Espín et al., 2016[3]; Cano et al., 2017[4]). These models aim to achieve the following four objectives: 1) improve patient experiences; 2) improve population health; 3) reduce the per capita cost of healthcare; and 4) improve the work-life balance of healthcare providers (i.e. the “Quadruple Aim” approach).
In 2000, the Spanish municipality of Badalona introduced an integrated care organisation responsible for providing health and social care. The remainder of this section outlines Badalona’s integrated care organisation – namely, the governance structure, service provision and delivery, as well as the supporting health information system.
Governance
Prior to 2000, health and social care services operated in silos within Badalona – the Badalona Healthcare Services (Badalona Serveis Assistencials, BSA) was responsible for healthcare, while the City Council operated social services. This arrangement led to service duplication and uncoordinated care delivery. In response, in 2000, the Badalona City Council agreed to merge health and social care services into one integrated health and social care organisation. This organisation goes by the name of BSA and is owned by the Badalona City Council (Piera, 2015[5]).
BSA’s governance structure supports several types of care integration within the health and social care system (Rossi Mori, Albano and Piera Jimenez, 2017[6]):
Functional integration: back office and support function co‑ordination across all units involved
Organisational integration: a single organisation in charge of health and social care provision
Professional integration: multidisciplinary teams of health and social care professionals across different tiers of care
Service/clinical integration: development of the care pathway as a single/seamless process across time, place and discipline
Normative integration: shared mission work values and organisational/professional culture
Systemic integration: alignment of incentives at organisational level.
“The governance model, involving all stakeholders and especially including policy leaders has provided organisational support, strong commitment and has enhanced a cohesive culture which set the basis for the continuum of the integrated care.” (Valls, Piera and Tolra, n.d.[7])
Service provision and delivery
BSA is responsible for providing a full spectrum of health and social care services to populations living in the northern metropolitan area of Barcelona including the cities of Badalona, Montgat and Tiana. That is, primary care, specialised care, intermediate care and home care (including social home care). These services are delivered within the Hospital Municipal de Badalona, the Homecare Integrated Service, the intermediate care centre “El Carme”, seven primary care centres and a Centre for Sexual and Reproductive Health (Valls, Piera and Tolra, n.d.[7]).
One of the key innovations to emerge from BSA is the “Care Model for Patients with Complex Chronic Conditions” (MAMCC). MAMCC follows a case management approach, which is led by both nurses and social workers who are at the centre of MAMCC. Case managers are responsible for co‑ordinating health professionals and service provision, as well as providing support to the patient and their family/carer. The case managers are situated mainly within the primary care sector, however, they have the ability to move across different care levels, including the patient’s home.
MAMCC encompasses a range of individual programs, which are outlined in Box 7.1. People are allocated to one or several programs based on a predictive modelling tool that stratifies patients into risk groups or via their healthcare provider.
At a high-level, MAMCC (Valls, Piera and Tolra, n.d.[7]):
Reshapes the care model so that is patient-focused
Identifies and prevents acute episodes to avoid unnecessary hospitalisations
Enables patients to benefit from individual integrated care plans
Promotes independent living
Provides better co‑ordination across healthcare professionals
Guarantees care continuity.
Box 7.1. Programs within the “Care Model for Patients with Complex Chronic Conditions” (MAMCC)
This box outlines programs within MAMCC – programs have been divided into EU-funded programs and home care programs, which are further split into health and social care.
EU-funded projects
ReAAL – telemonitoring programme for chronic diseases
Beyond Silos – short-term rehabilitation at home after injury or illness
Mastermind – Computerised Cognitive Behavioural Therapy for depression
Do Change – management of cardiac patients with new devices and behaviour change
UseCare
Home care programs – healthcare
Early discharge programme (HaD) – offers patients who have just undergone surgery home care for six weeks
Home hospitalisation – short follow-up at home after discharge from intermediate care centre
Palliative care at home (PADES) delivered by a geriatrician and nurse
AtDom programme – ongoing assistance at home
Regional case management for all types of chronic conditions
Telemonitoring to support management of chronic diseases
Home care programs – social care
Help at home
Meals at home
Cleaning at home
Home repairs
GPS tracking system
Social isolation and exclusion avoidance
Source: RossMori and Piera-Jiménez (2021[8]), “Collection of the Service Deployment Outlines about 20 Integrated Care initiatives in Badalona (2003‑15)”; RossiMori et al. (2019[9])), “A systematic analysis of the multi‑annual journey of Badalona towards integrated care”, http://doi.org/10.5334/ijic.s3344.
Health information system support
Large‑scale, population-based integrated care models require support from sophisticated health information systems. A list of IT tools used to support BSA is below (Valls, Piera and Tolra, n.d.[7]):
A longitudinal Integrated Care Record specific to BSA that is designed to manage and integrate health and social services was developed to improve communication across providers. The Integrated Care Record brings together data collected across all levels of health and social care. Nevertheless, systems to upload patient data differ across providers making it difficult to readily identify patient data.
The BSA Integrated Care Record is compatible with the Catalan Shared Medical Record (HC3). HC3 collects and stores information about the patient’s status and progress whilst receiving care. HC3 ensures there is interoperability of Integrated Care Records across public health providers for the whole region of Catalonia.
The Integrated Care Record System provides health and social care providers (including third sector care providers) with access to patient information.
OECD Best Practices Framework assessment
This section analyses BSA against the five criteria within OECD’s Best Practice Identification Framework – Effectiveness, Efficiency, Equity, Evidence‑base and Extent of coverage (see Box 7.2 for a high-level assessment). Further details on the OECD Framework can be found in Annex A.
Box 7.2. Assessment of BSA
Effectiveness
An evaluation of BSA as a whole is not available, instead evaluations have focused on individual programs
Evaluations from individual programs show they reduce healthcare use and improve patient satisfaction
Efficiency
Similar to “Effectiveness”, an evaluation of BSA’s efficiency as a whole is not available
Cost-utility analyses of individual programme that make up BSA indicate they are cost-effective, and in certain cases, cost-saving
Equity
Programs that address the needs of disadvantaged groups are developed and implemented on an ad hoc basis. For example, BSA administrators implemented a programme to encourage people within the Pakistani community to have a check-up due to high rates of untreated diabetes.
Evidence‑base
The quality of evidence supporting the effectiveness and efficiency of BSA shows mixed results when using the Effective Public Health Practice Project’s quality assessment tool for quantitative studies
In general, studies evaluating BSA performed well in terms of reducing selection bias, the choice of study design and limiting withdrawals and dropouts
Extent of coverage
BSA is a population based integrated care organisation, therefore it services cover the whole population
Effectiveness
There has been no evaluation of BSA as a whole to date. Therefore, this section measures BSA’s effectiveness according to individual programs that make up the integrated care organisation (see Box 7.1). Specifically, it focuses on two programs – regional case management programs and the early discharge programme. These were chosen given they are both major programs within BSA and have good available data.
Regional case management programs for patients with chronic health conditions led to a (Vela et al., 2018[10]; Lasmarías et al., 2018[11]):
8% reduction in formal care
40% reduction in emergencies
56% reduction in non-programmed hospital admissions
89% increase in patient satisfaction with service provision
59% increase in home‑assisted deaths.
Early discharge programme for patients who have just undergone surgery (Santaeugènia et al., 2013[12]; Mas and Inzitari, 2012[13]; Closa et al., 2017[14]; Mas and Santaeugènia, 2015[15]):
67% increase in patients completing rehabilitation (specifically, among those aged 70‑83 years of age)
28% reduction in relapse
50% reduction in rehabilitation
27% decline in mortality rates.
Efficiency
Similar to “Effectiveness”, an evaluation measuring the efficiency of BSA is not available. For this reason, this section summarises key findings from efficiency studies, which are available for three individual programs (see Box 7.1).
Super@ (Spanish version of the EU project, Mastermind, a Computerised Cognitive Behavioural Therapy for depression) (Vis et al., 2015[16]):
Super@ recorded an incremental cost-effectiveness ratio (ICER) of EUR 29 367 per quality-adjusted life year (QALY) when using a discount rate of 3%. The ICER declined to EUR 26 484 when not discounted. Both figures fall under the commonly applied cost-effectiveness threshold of EUR 30 000 used in Spain (Piera-Jiménez et al., 2021[17]).
BeyondSilos, a telehealth-enhanced integrated care model in the domiciliary setting for older patients (Piera-Jiménez et al., 2020[18]):
The intervention recorded an ICER per QALY of EUR 6 506, which is below the commonly applied EUR 30 000 cost-effectiveness threshold
Do CHANGE, management of cardiac patients with new devices and behaviour change:
Do Change recorded a negative ICER per QALY in Spain (EUR ‑2 515) indicating the intervention is not only cost-effective, but also cost saving. The intervention is also cost-effective, although not cost-saving, in other countries including the Netherlands (EUR 1 374) (Piera-Jiménez et al., 2020[19]).
Equity
BSA addresses the needs of disadvantaged groups on an ad-hoc basis. For example, BSA administrators identified that members of the region’s Pakistan community had higher rates of untreated diabetes leading to worse health outcomes (e.g. diabetic comas). This was due to genetic factors and a cultural tradition of proactively seeking healthcare. In response, BSA administrators took the following action: 1) placing mediators within primary care centres to facilitate discussions between GPs and patients within the community, 2) seeking the assistance of the Mosque’s imam to raise the issue during sermons, and 3) developing flyers in the local language encouraging people to have a health check-up.
People with a lower socio-economic status are more likely to live with complex health needs, indicating the integrated care model may reduce inequalities. Socio-economic status is a key predictor of health status, for example, analysis of Eurostat data by OECD found men in the most deprived group are 1.5 times more likely to be obese than those in the least deprived group, with this figure increasing to 1.9 for women (OECD, 2019[20]). Poor lifestyle behaviours contribute to higher rates of multimorbidity, which is reflected by data from Spain. For example, 12% of the Spanish population live with obesity in the top income quintile compared to 17% in the lowest income quintile (Eurostat, 2019[21]). By developing a model to improve the level of care delivered to patients with complex health needs, health inequalities can be reduced, however, a specific analysis examining this topic is not available.
Evidence‑based
The “Evidence‑based” criterion assesses the quality of evidence used to measure effectiveness, efficiency and equity. That is, three recent studies by Piera-Jiménez – (Piera-Jiménez et al., 2021[17]), (Piera-Jiménez et al., 2020[18]) and (Piera-Jiménez et al., 2020[19]). Each of the three studies were assessed using the Effective Public Health Practice Project’s quality assessment tool for quantitative studies (1998[22]). This tool examines several factors that can bias results such as the study design and level of withdrawals and dropouts. Findings from each assessment are in Table 7.1, which show mixed results across the three studies.
Table 7.1. Evidence‑based assessment – BSA
|
Assessment category |
Question |
Rating for (Piera-Jiménez et al., 2021[17]) measuring the impact of the Super@ intervention |
Rating for (Piera-Jiménez et al., 2020[18]) measuring the impact of the BeyondSilos intervention |
Rating for (Piera-Jiménez et al., 2020[19]) measuring the impact of the Do CHANGE intervention |
|---|---|---|---|---|
|
Selection bias |
Are the individuals selected to participate in the study likely to be representative of the target population? |
Somewhat likely |
Very likely |
Very likely |
|
What percentage of selected individuals agreed to participate? |
80‑100% |
60‑79% |
Less than 60% |
|
|
Selection bias score: |
Strong |
Moderate |
Weak |
|
|
Study design |
Indicate the study design |
Pragmatic within group trial |
Observational prospective cohort study |
RCT |
|
Was the study described as randomised? |
No |
No |
Yes |
|
|
Was the method of randomisation described? |
N/A |
N/A |
Yes |
|
|
Was the method of randomisation appropriate? |
N/A |
N/A |
Yes |
|
|
Study design score: |
Moderate |
Moderate |
Strong |
|
|
Confounders |
Were there important differences between groups prior to the intervention? |
Can’t tell |
Yes |
No |
|
What percentage of potential confounders were controlled for? |
80‑100% |
80‑100% |
N/A |
|
|
Confounders score: |
Moderate |
Strong |
Strong |
|
|
Blinding |
Was the outcome assessor aware of the intervention or exposure status of participants? |
Yes |
Yes |
Yes |
|
Were the study participants aware of the research question? |
Yes |
Can’t tell |
Yes |
|
|
Blinding score: |
Weak |
Weak |
Weak |
|
|
Data collection methods |
Were data collection tools shown to be valid? |
Can’t tell |
Yes |
Can’t tell |
|
Were data collection tools shown to be reliable? |
Can’t tell |
Can’t tell |
Can’t tell |
|
|
Data collection methods score: |
Weak |
Moderate |
Weak |
|
|
Withdrawals and dropouts |
Were withdrawals and dropouts reported in terms of numbers and/or reasons per group? |
Yes |
Yes |
Yes |
|
Indicate the percentage of participants who completed the study? |
60‑79% |
80‑100% |
80‑100% |
|
|
Withdrawals and dropouts score: |
Moderate |
Strong |
Strong |
Note: N/A = not applicable.
Source: Effective Public Health Practice Project (1998[22]), “Quality assessment tool for quantitative studies”, https://www.nccmt.ca/knowledge-repositories/search/14.
Extent of coverage
BSA’s predictive modelling tool enables BSA to deliver integrated care across the covered population. BSA currently offers health and social care services to people residing in the municipalities and town of Badalona, Montgat and Tiana. Using electronic patient data, the whole population is stratified into risk groups with those considered to have complex health needs eligible for MAMCC (Care Model for Patients with Complex Chronic Conditions) (see “Intervention description”). As outlined under “Equity”, the predictive tool is therefore able to deliver tailored care to the whole population, including disadvantaged groups (e.g. those with a low socio-economic status).
Policy options to enhance performance
In this section, recommendations are given for BSA administrators, as well as policy makers in other countries who are considering implementing a similar model of care, as to how the performance of the programme could be further enhanced.
Enhancing effectiveness
Ensure health professionals have the skills and motivation to deliver multidisciplinary care. MAMCC led to the emergence of new professional roles, as well as changed how work is organised and performed among existing health professionals. Although these changes align with international best practice, they nonetheless “generated resistance and conflict among professionals” (Vallve et al., 2016[23]). For this reason, before implementing any model of care, it is important health professionals receive training on how to work as a team. Ideally training would be harmonised and delivered as part of the formal curricula. Although training is important, many skills are learnt “on the job”. Such knowledge can be shared by establishing “learning networks” among health professionals – e.g. via webinars, conferences, materials and guidebooks.
“… domiciliary care has also brought resistances among medical staff. Domiciliary attention requires a new vision of care, which not all doctors are prepared to give. Besides, the new teams of homecare attention imply that patients change doctor when they start to be attended at home, and some of the doctors perceive it as an intrusion and don’t agree with their patients being attended by another professional.”” (Vallve et al., 2016[23])
Involve health and social care providers when developing and implementing a new model of care. As outlined by Vallve et al. (2016[23]), despite ongoing communication with providers, many still resist this new model of care. Given workforce support is crucial for success and sustainability, it is important they are involved in the transformation process from the outset.
“There have been many meetings with social workers from the city council explaining the benefits of the model but, although it’s been 12 years since it was implemented, according to some of the interviewees some of these resistances still prevail.” (Vallve et al., 2016[23])
Co‑ordinate health information systems across health and social care providers. Large‑scale integrated care models must be supported by sophisticated health information systems – e.g. to share patient data electronically. As outlined under the “Intervention description”, EHRs specific to the municipality of Badalona exist, however, providers use different information systems to upload patient data. As a consequence it can be difficult for health professionals to readily identify patient information. Policy makers should therefore focus on aligning health information systems across the spectrum of care.
“Another problem we have is related to software, which is dreadful. Look, at the hospital they work with a software called GESDOHC. Primary care centres have another programme called ECAP and at “El Carme” (the intermediate care centre) they use another programme. So, you can imagine. Doctors come around and say they don’t find the information from the specialist and ask you to look for it. There are many programs, and it is complicated for us, because we are the link among all of them. And still, at the ECAP you may find all the information from Can Ruti (the hospital from ICS operating at the area of Badalona), and we also have to look at it, because many patients go there…”
Enhancing efficiency
Efficiency is a measure of effectiveness in relation to inputs used. Therefore, interventions that increase effectiveness without significant increases in costs, or reduce costs while keeping effectiveness at least constant, have a positive effect on efficiency.
Enhancing equity
Develop permanent programs dedicated to the needs of disadvantaged groups. Individual programs that make up BSA (Box 7.1) address the population as a whole. As outlined under “Equity”, the specific needs of disadvantaged groups – e.g. low socio-economic status, migrants – are taken into account on an ad hoc basis. Developing permanent individual programs targeting disadvantaged groups can help reduce health inequalities. For example, the OptiMedis population integrated care organisation in Germany has a dedicated Health Kiosk that caters to the needs of migrants by offering counselling services in a range of languages including Arabic, Farsi, Russian and Polish.
Improve access to healthcare services for disadvantaged groups by promoting health literacy. Disadvantaged groups, such as those with a lower socio-economic status, are less likely to access necessary healthcare services (OECD, 2019[24]). For example, across the OECD, 74% of people in the highest income quintile have been screened for breast cancer compared to 63% among those in the lowest income quintile (OECD, 2019[24]). Although disadvantaged groups stand to benefit most from integrated care models, which incentivises high-quality, preventative care, they may be less likely to access these services. Programs that promote health literacy among disadvantaged groups may increase access to healthcare services (see Box 7.3 for further details).
Box 7.3. Building population health literacy
Recent analysis estimated that more than half of OECD countries with available data had low levels of HL. To address low rates of adult health literacy, OECD have outlined a four‑pronged policy approach, which align:
Strengthen the health system role: establish national strategies and framework designed to address HL
Acknowledge the importance of HL through research: measure and monitor the progress of HL interventions to better understand what policies work
Improve data infrastructure: improve international comparisons of HL as well as monitoring HL levels over time
Strengthen international collaboration: share best practice interventions to boost HL across countries.
Source: OECD (2018[25]), “Health literacy for people‑centred care: Where do OECD countries stand?”, https://doi.org/10.1787/d8494d3a-en.
Enhancing the evidence‑base
Undertake research to identify the optimal combination of programs to support patients with complex health needs. To date, research has focused on the effectiveness of individual programs within BSA’s integrated care organisation (see Box 7.1) (Rossi Mori, Albano and Piera Jimenez, 2017[6]). Given patients likely access more than just one programme, it is important to understand the impact of different programs when combined (e.g. do they have a more than additive effect on patient outcomes?). Results from the analysis will help optimise care for patients with complex health needs.
Studies evaluating the impact of BSA as a whole would strengthen the evidence‑base. In addition to examining individual programs (and the combination of them), it is important to evaluate the impact of BSA as a whole. Key indicators to measure include: hospitalisations, emergency department visits, visits to a GP, patient quality of life (e.g. EQ‑5D), and clinical outcomes (e.g. risk factors, mortality, disease incidence). OECD are currently piloting a range of integrated care model indicators – these cover all-cause and disease‑specific hospital admissions, all-cause mortality after hospital discharge and prescription of appropriate medication for secondary prevention after hospital discharge (Barrenho et al., 2022[26]). In addition to an outcome/effectiveness evaluation, it is important to evaluate the overall efficiency of BSA using a cost-effectiveness, cost-benefit, or cost-utility analysis. Demonstrating an intervention is efficient is crucial for maintaining long-term political support.
Enhancing extent of coverage
No policy options are recommended for enhancing the extent of coverage given BSA covers the whole population. However, improving access to care for disadvantaged populations will ultimately increase the reach of this care model (see “Enhancing equity”).
Transferability
This section explores the transferability of BSA and is broken into three components: 1) an examination of previous transfers; 2) a transferability assessment using publicly available data; and 3) additional considerations for policy makers interested in transferring BSA.
Previous transfers
BSA exists solely within a selection of towns and municipalities in Spain, nevertheless, similar models of care are increasingly popular among OECD countries. For example:
OECD’s report on primary care (2020[27]) identified 17 member countries which have developed “new models of primary care”,1 that deliver integrated care to patients.
The European Commission funded ICARE4U project related to multimorbid patients identified 101 models of integrated care across 24 European countries, of which 40% target those aged 65+ (Melchiorre et al., 2020[28]).
BSA administrators have highlighted several transfer facilitators associated with integrated care models combining health and social care. These are listed in Box 7.4.
Box 7.4. Transfer facilitators
This box outlines facilitators for transferring integrated care models that bring together health and social care. The list is drawn from existing references, which are listed at the bottom of this box. The facilitators are broken into four categories: policy, governance, workforce and culture and digital tools.
Policy
Strong policy commitment towards providing patient-centric care
Ensure the views of all key stakeholders are included – e.g. research organisations, policy makers, service providers and end-users
Governance
One governance and organisational structure for health and social care services – without such a structure, implementation costs are likely to be very high given the change required for institutional, organisation, cultural and legal arrangements
Implementation is more straightforward in countries with national health systems as opposed to insurance‑based models
Involvement of as many stakeholders as possible in terms of horizontal governance
Workforce and culture
Allowing health and social care providers to play a leading role in developing and implementing this new model of care
Willingness and motivation among the workforce to implement such models of care
Culture of innovation
Involvement of young people given they have a tendency to be more innovative, experience less cultural constraints and have good ideas
Digital tools
Sophisticated health information system, including wide‑spread use of EHRs that allow for efficient communication across the spectrum of care
No resistance to health technology among patients and providers
Source: Vallis, Piera and Tolra (n.d.[7]), “Report of in depth analysis of Badalona Healthcare services (BSA)” case study”; Vallive et al. (2016[23]), “SELFIE 2020: Work Package 2: Thick descriptions of the two Catalan case studies, Badalona Serveis Assistencials (BSA) (Spain)”; Lupiañez-Villanueva and Theben (2015[29]), “Strategic Intelligence Monitor on Personal Health Systems Phase 3 (SIMPHS3): BSA (Spain) Case Study Report”.
Transferability assessment
This section outlines the methodological framework to assess transferability followed by analysis results.
Methodological framework
A few indicators to assess the transferability of BSA were identified (see Table 7.2). Indicators were drawn from international databases and surveys to maximise coverage across OECD and non-OECD European countries. Please note, the assessment is intentionally high level given the availability of public data covering OECD and non-OECD European countries. For further details on the methodology used, see Annex A.
Table 7.2. Indicators to assess transferability – BSA
|
Indicator |
Reasoning |
Interpretation |
|---|---|---|
|
Population context |
||
|
% of older individuals who sought health information online in the past 3 months |
The intervention utilises digital tools to engage with participants – e.g. electronic health records |
🡹 value = more transferable |
|
Sector context (health and social care) |
||
|
Proportion of GPs who work in single‑handed practices |
The intervention is more transferable in countries where GPs feel comfortable working with other health professionals. This indicator is a proxy to measure the willingness of GPs to work in co‑ordinated teams. |
Low = more transferable High = less transferable |
|
Proportion of physicians in primary care facilities using electronic health records |
EHRs improve the ability of health professionals to provide integrated patient-centred care. Therefore, the intervention is more transferable in countries that utilise EHRs in primary care facilities. |
🡹 value = more transferable |
|
Proportion of hospitals using electronic patient records for inpatients |
As above |
🡹 value = more transferable |
|
The extent of task shifting between physicians and nurses in primary care |
This intervention promotes integrated care provided by multidisciplinary teams. Therefore, the intervention is more transferable in countries where physicians feel comfortable shifting tasks to nurses. |
The more “extensive” the more transferable |
|
The use of financial incentives to promote co‑ordination in primary care |
The intervention is more transferable to countries with financial incentives that promote co‑ordination of care across health professionals. |
Bundled payments or co‑ordinated payment = more transferable |
|
Economic context |
||
|
Primary healthcare expenditure as a percentage of current health expenditure |
The intervention places a stronger emphasis on primary care, therefore, it is likely to be more successful in countries that allocate a higher proportion of health spending to primary care |
🡹 value = more transferable |
Source: WHO (2018[30]), “Primary Health Care (PHC) Expenditure as percentage Current Health Expenditure (CHE)”, https://apps.who.int/nha/database; Oderkirk (2017[31]), “Readiness of electronic health record systems to contribute to national health information and research”, https://dx.doi.org/10.1787/9e296bf3-en; Schäfer et al. (2019[32]), “Are people’s health care needs better met when primary care is strong? A synthesis of the results of the QUALICOPC study in 34 countries”, https://doi.org/10.1017/S1463423619000434; Maier and Aiken (2016[33]), “Task shifting from physicians to nurses in primary care in 39 countries: a cross-country comparative study”, https://doi.org/10.1093/eurpub/ckw098; OECD (2020[27]), Realising the Potential of Primary Healthcare, https://doi.org/10.1787/a92adee4-en; OECD (2016[34]), “Health Systems Characteristics Survey”, https://qdd.oecd.org/subject.aspx?Subject=hsc; European Observatory on Health Systems and Policies (2021[35]), “The Health Systems and Policy Monitor”, https://eurohealthobservatory.who.int/countries/overview.
Table 7.3. Transferability assessment by country (OECD and non-OECD European countries) – BSA
A darker shade indicates BSA is more suitable for transferral in that particular country
|
Country |
% older people using the internet for health information |
% GPs in single practices |
% PC* using EHRs |
% hospitals using EHRs |
Task shifting in PC* |
Financial incentives |
Primary expenditure percentage CHE** |
|---|---|---|---|---|---|---|---|
|
Spain |
41 |
Low |
99 |
80 |
Limited |
No incentive |
39 |
|
Australia |
n/a |
Low |
96 |
20 |
Extensive |
Bundled |
37 |
|
Austria |
32 |
High |
80 |
99 |
None |
Co‑ordinated payment |
37 |
|
Belgium |
37 |
High |
n/a |
n/a |
Limited |
Bundled |
40 |
|
Bulgaria |
12 |
High |
n/a |
n/a |
None |
Bundled |
47 |
|
Canada |
n/a |
Low |
77 |
69 |
Extensive |
Bundled |
48 |
|
Chile |
n/a |
n/a |
65 |
69 |
n/a |
No incentive |
n/a |
|
Colombia |
n/a |
n/a |
n/a |
n/a |
n/a |
No incentive |
n/a |
|
Costa Rica |
n/a |
n/a |
n/a |
n/a |
n/a |
No incentive |
33 |
|
Croatia |
18 |
n/a |
3 |
n/a |
Limited |
No incentive |
38 |
|
Cyprus |
36 |
Low |
n/a |
n/a |
Limited |
No incentive |
41 |
|
Czech Republic |
41 |
High |
n/a |
100 |
None |
No incentive |
33 |
|
Denmark |
56 |
Medium |
100 |
100 |
Limited |
Co‑ordinated payment |
38 |
|
Estonia |
32 |
High |
99 |
100 |
Limited |
No incentive |
44 |
|
Finland |
60 |
Medium |
100 |
100 |
Extensive |
No incentive |
46 |
|
France |
39 |
n/a |
80 |
60 |
None |
Bundled |
43 |
|
Germany |
55 |
High |
n/a |
n/a |
None |
Co‑ordinated payment |
48 |
|
Greece |
20 |
High |
100 |
50 |
None |
No incentive |
45 |
|
Hungary |
42 |
High |
n/a |
n/a |
Limited |
No incentive |
40 |
|
Iceland |
56 |
Low |
100 |
100 |
Limited |
Co‑ordinated payment |
35 |
|
Ireland |
40 |
Low |
95 |
35 |
Extensive |
No incentive |
47 |
|
Israel |
n/a |
n/a |
100 |
100 |
n/a |
Co‑ordinated payment |
n/a |
|
Italy |
27 |
Medium |
n/a |
n/a |
Limited |
Bundled |
n/a |
|
Japan |
n/a |
n/a |
36 |
34 |
n/a |
No incentive |
52 |
|
Korea |
n/a |
n/a |
n/a |
n/a |
n/a |
No incentive |
57 |
|
Latvia |
28 |
High |
70 |
90 |
Limited |
Bundled |
39 |
|
Lithuania |
31 |
Medium |
n/a |
n/a |
Limited |
No incentive |
48 |
|
Luxembourg |
46 |
Medium |
n/a |
n/a |
None |
No incentive |
38 |
|
Malta |
34 |
Medium |
n/a |
n/a |
Limited |
No incentive |
62 |
|
Mexico |
n/a |
n/a |
30 |
49 |
n/a |
Co‑ordinated payment |
44 |
|
Netherlands |
67 |
Medium |
n/a |
n/a |
Extensive |
Bundled |
32 |
|
New Zealand |
n/a |
Low |
95 |
100 |
Extensive |
No incentive |
n/a |
|
Norway |
52 |
Low |
100 |
100 |
None |
No incentive |
39 |
|
Poland |
25 |
Medium |
30 |
10 |
None |
No incentive |
47 |
|
Portugal |
19 |
Low |
n/a |
n/a |
Limited |
No incentive |
58 |
|
Romania |
17 |
Medium |
n/a |
n/a |
None |
No incentive |
35 |
|
Slovak Republic |
39 |
High |
89 |
100 |
None |
No incentive |
n/a |
|
Slovenia |
30 |
High |
n/a |
n/a |
Limited |
No incentive |
43 |
|
Sweden |
44 |
Low |
100 |
100 |
Limited |
Co‑ordinated payment |
n/a |
|
Switzerland |
57 |
Medium |
40 |
100 |
None |
No incentive |
40 |
|
Türkiye |
11 |
Low |
n/a |
n/a |
None |
No incentive |
n/a |
|
United Kingdom |
45 |
Low |
99 |
100 |
Extensive |
No incentive |
53 |
|
United States |
n/a |
n/a |
83 |
76 |
Extensive |
No incentive |
n/a |
Note: *PC = primary care. **CHE = current health expenditure. n/a = no data available.
Source: See Table 7.2.
To help consolidate findings from the transferability assessment above, countries have been clustered into one of three groups, based on indicators reported in Table 7.2. Countries in clusters with more positive values have the greatest transfer potential. For further details on the methodological approach used, please refer to Best Practice case study guide.
Key findings from each of the clusters are below with further details in Figure 7.1 and Table 7.4:
Countries in cluster one typically have populations where internet use for healthcare purposes is high. Given the integrated care model incorporates various digital tools, this may indicate higher levels of engagement from the population. However, expenditure on primary care is relatively low in these countries indicating potential long-term affordability issues. Spain, where this model of care operates, is in this cluster, meaning conditions in which these clusters could improve on, although ideal, are not pre‑requisites.
Countries in cluster two should first establish whether its health and social care system is ready to transfer this intervention – e.g. will healthcare professionals be accepting of working as a multidisciplinary care team? This model of care is likely to be popular among the population given relatively high levels of digital health literacy, further, countries in these cluster spend relatively more on primary care indicating support for proactive (preventative) style care.
Unlike countries in cluster two, countries in cluster three have systems in place to support integrated care models within the health and social system. Nevertheless, digital interventions may be less successful among these countries given lower levels of digital health literacy.
Figure 7.1. Transferability assessment using clustering – BSA
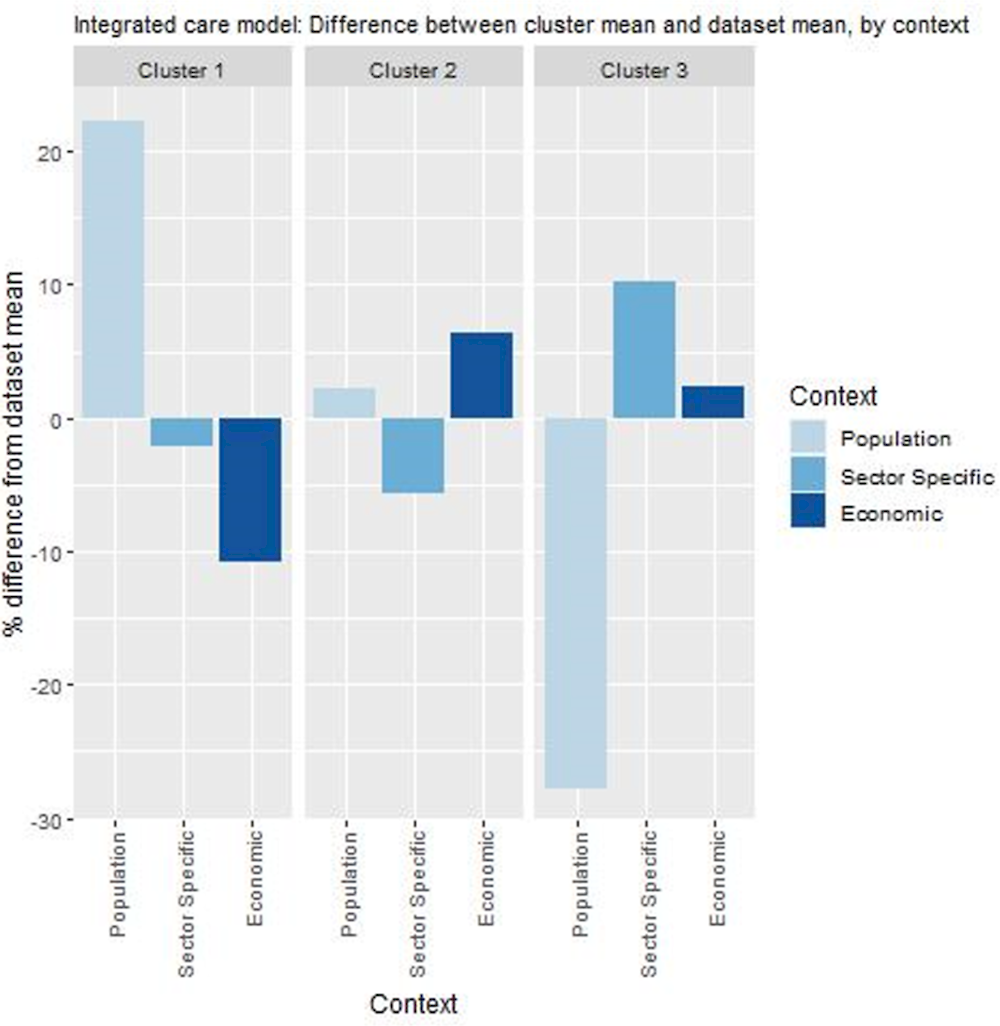
Note: Bar charts show percentage difference between cluster mean and dataset mean, for each indicator.
Table 7.4. Countries by cluster – BSA
|
Cluster 1 |
Cluster 2 |
Cluster 3 |
|---|---|---|
|
Cyprus Denmark Germany Iceland Malta New Zealand Norway Portugal Spain Sweden United Kingdom |
Australia Bulgaria Canada Czech Republic Finland France Greece Ireland Luxembourg Netherlands Poland Romania Slovak Republic Switzerland |
Austria Belgium Croatia Estonia Hungary Italy Latvia Lithuania Mexico Slovenia |
Note: Due to high levels of missing data, the following countries were omitted from the analysis: Chile, Colombia, Costa Rica, Israel, Japan, Korea, Türkiye and the United States.
New indicators to assess transferability
Data from publicly available datasets alone is not ideal to assess the transferability of public health interventions. Box 7.5 outlines several new indicators policy makers could consider before transferring BSA.
Box 7.5. New indicators, or factors, to consider when assessing transferability – BSA
In addition to the indicators within the transferability assessment, policy makers are encouraged to collect information for the following indicators:
Population context
What is the population’s attitude towards receiving care from health professionals who are not doctors?
What is the level of health literacy among patients? (i.e. are patients likely to engage in shared decision-making?)
Sector specific context (health and social care)
Does the healthcare workforce support care integration and co‑ordination?
Is there a culture of change and innovation among health and social care professionals?
Do regulatory arrangements support care integration across and within health and social care services?
Does the clinical information system support: a) sharing of patient data across health professionals? b) Sharing of patient data across health and social care facilities?
Do health provider reimbursement schemes support co‑ordinated care? (E.g. bundled payments, add-on payments that incentivise co‑ordinated care)
Are health and social care professionals digitally health literate?
How are health and social care services currently provided?*
Political context
Has the intervention received political support/commitment from key decision-makers? (E.g. a national strategy to address ageing and chronicity)
Has the intervention received commitment from key decision-makers?
Economic context
What is the cost of implementing and operating the intervention in the target setting?
* This model of care more easily transferable to healthcare systems with a national health system model when compared to insurance‑based models.
Conclusion and next steps
BSA is an integrated care organisation owned by the Badalona City Council. Unlike many integrated care organisations, BSA brings together both health and social care services to better meet the needs of the population. BSA supports various levels of integration including organisational, functional, clinical and professional.
Individual programs within BSA have demonstrated both effectiveness and efficiency. An evaluation measuring the overall effectiveness and efficiency of BSA is not available. However, certain individual programs that make up BSA show they reduce healthcare utilisation, improve patient outcomes and are cost-effective.
The needs of disadvantaged groups are addressed on an ad hoc basis. Individual programs delivered as part of BSA address the population as a whole. Nevertheless, specific programs are developed on an ad hoc basis in response to unmet needs from disadvantaged groups. For example, BSA administrators introduced several strategies to combat high rates of untreated diabetes in the Pakistani community.
BSA aligns with international best practice, nevertheless, there are opportunities for it to further improve. For example, ongoing training to ensure health and social care professionals have the skills, confidence and motivation to work as a multidisciplinary team will ultimately improve service delivery. Further, future research projects should focus on evaluating BSA as a whole as opposed to focusing on individual programs.
Countries interested in transferring BSA must first consider the context in which their health and social care systems operate. The ability for countries to integrated health and social care services will depend on how both sectors are currently organised. Key transfer facilitates include, but are not limited to, a sophisticated health information system, a motivated workforce and strong political commitment.
Box 7.6. Next steps for policy makers and funding agencies – BSA
Next steps for policy makers and funding agencies to enhance BSA are listed below:
Consider policy options in this case study to further enhance BSA’s performance
Share key transfer facilitators with policy makers interested in developing an integrated care organising combining both health and social care
Focus future research efforts on the impact of BSA as a whole given the growing interested in such models of care across OECD and EU27 countries.
References
[26] Barrenho, E. et al. (2022), “International comparisons of the quality and outcomes of integrated care: Findings of the OECD pilot on stroke and chronic heart failure”, OECD Health Working Papers, No. 142, OECD Publishing, Paris, https://doi.org/10.1787/480cf8a0-en.
[4] Cano, I. et al. (2017), “Protocol for regional implementation of community-based collaborative management of complex chronic patients”, npj Primary Care Respiratory Medicine, Vol. 27/1, https://doi.org/10.1038/s41533-017-0043-9.
[14] Closa, C. et al. (2017), “Hospital-at-home Integrated Care Program for Older Patients With Orthopedic Processes: An Efficient Alternative to Usual Hospital-Based Care”, Journal of the American Medical Directors Association, Vol. 18/9, pp. 780-784, https://doi.org/10.1016/j.jamda.2017.04.006.
[3] Dueñas-Espín, I. et al. (2016), “Proposals for enhanced health risk assessment and stratification in an integrated care scenario”, BMJ Open, Vol. 6/4, p. e010301, https://doi.org/10.1136/bmjopen-2015-010301.
[22] Effective Public Health Pratice Project (1998), Quality assessment tool for quantitative studies, https://www.nccmt.ca/knowledge-repositories/search/14.
[35] European Observatory on Health Systems and Policies (2021), The Health Systems and Policy Monitor, https://eurohealthobservatory.who.int/countries/overview (accessed on 9 June 2021).
[1] Eurostat (2022), People having a long-standing illness or health problem, by sex, age and income quintile.
[21] Eurostat (2019), Body mass index (BMI) by sex, age and educational attainment level.
[11] Lasmarías, C. et al. (2018), “Development and implementation of an advance care planning program in Catalonia, Spain”, Palliative and Supportive Care, Vol. 17/04, pp. 415-424, https://doi.org/10.1017/s1478951518000561.
[29] Lupiañez-Villanueva, F. and A. Theben (2015), Strategic Intelligence Monitor on Personal Health Systems Phase 3 (SIMPHS3): BSA (Spain) Case Study Report.
[33] Maier, C. and L. Aiken (2016), “Task shifting from physicians to nurses in primary care in 39 countries: a cross-country comparative study”, The European Journal of Public Health, Vol. 26/6, pp. 927-934, https://doi.org/10.1093/eurpub/ckw098.
[13] Mas, M. and M. Inzitari (2012), “A Critical Review of Early Supported Discharge for Stroke Patients: From Evidence to Implementation into Practice”, International Journal of Stroke, Vol. 10/1, pp. 7-12, https://doi.org/10.1111/j.1747-4949.2012.00950.x.
[15] Mas, M. and S. Santaeugènia (2015), “Hospitalización domiciliaria en el paciente anciano: revisión de la evidencia y oportunidades de la geriatría”, Revista Española de Geriatría y Gerontología, Vol. 50/1, pp. 26-34, https://doi.org/10.1016/j.regg.2014.04.003.
[28] Melchiorre, M. et al. (2020), “Integrated Care Programs for People with Multimorbidity in European Countries: eHealth Adoption in Health Systems”, BioMed Research International, Vol. 2020, pp. 1-23, https://doi.org/10.1155/2020/9025326.
[2] Monterde, D. et al. (2020), “<p>Performance of Comprehensive Risk Adjustment for the Prediction of In-Hospital Events Using Administrative Healthcare Data: The Queralt Indices</p>”, Risk Management and Healthcare Policy, Vol. Volume 13, pp. 271-283, https://doi.org/10.2147/rmhp.s228415.
[31] Oderkirk, J. (2017), “Readiness of electronic health record systems to contribute to national health information and research”, OECD Health Working Papers, No. 99, OECD Publishing, Paris, https://doi.org/10.1787/9e296bf3-en.
[27] OECD (2020), Realising the Potential of Primary Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/a92adee4-en.
[24] OECD (2019), Health for Everyone?: Social Inequalities in Health and Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/3c8385d0-en.
[20] OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/67450d67-en.
[25] OECD (2018), “Health literacy for people-centred care: Where do OECD countries stand?”, OECD Health Working Papers, No. 107, OECD Publishing, Paris, https://doi.org/10.1787/d8494d3a-en.
[34] OECD (2016), Health Systems Characteristics Survey 2016, https://qdd.oecd.org/subject.aspx?Subject=hsc.
[5] Piera, J. (2015), Una realtà innovativa di integrazione sociosanitaria: l’esperenzia della BSA, Badalona Serveis Assistencials, Catalonia.
[18] Piera-Jiménez, J. et al. (2020), “BeyondSilos, a Telehealth-Enhanced Integrated Care Model in the Domiciliary Setting for Older Patients: Observational Prospective Cohort Study for Effectiveness and Cost-Effectiveness Assessments”, JMIR Medical Informatics, Vol. 8/10, p. e20938, https://doi.org/10.2196/20938.
[17] Piera-Jiménez, J. et al. (2021), “Guided Internet-Based Cognitive Behavioral Therapy for Depression: Implementation Cost-Effectiveness Study”, Journal of Medical Internet Research, Vol. 23/5, p. e27410, https://doi.org/10.2196/27410.
[19] Piera-Jiménez, J. et al. (2020), “Changing the Health Behavior of Patients With Cardiovascular Disease Through an Electronic Health Intervention in Three Different Countries: Cost-Effectiveness Study in the Do Cardiac Health: Advanced New Generation Ecosystem (Do CHANGE) 2 Randomized Controlled Trial”, Journal of Medical Internet Research, Vol. 22/7, p. e17351, https://doi.org/10.2196/17351.
[6] Rossi Mori, A., V. Albano and J. Piera Jimenez (2017), “Badalona Story: integrating the integration initiatives”, International Journal of Integrated Care, Vol. 17/5, p. 315, https://doi.org/10.5334/ijic.3632.
[9] RossiMori, A. et al. (2019), “A systematic analysis of the multi-annual journey of Badalona towards integrated care”, International Journal of Integrated Care, Vol. 19/4, p. 344, https://doi.org/10.5334/ijic.s3344.
[8] RossiMori, A. and J. Piera-Jiménez (2021), Collection of the Service Deployment Outlines about 20 Integrated Care initiatives in Badalona (2003-2015).
[12] Santaeugènia, S. et al. (2013), “Direct Admission to Intermediate Care for Older Adults With Reactivated Chronic Diseases: Avoiding Both Conventional Hospitalization and Emergency Department Use?”, Journal of the American Medical Directors Association, Vol. 14/6, pp. 444-445, https://doi.org/10.1016/j.jamda.2013.02.013.
[32] Schäfer, W. et al. (2019), “Are people’s health care needs better met when primary care is strong? A synthesis of the results of the QUALICOPC study in 34 countries”, Primary Health Care Research & Development, Vol. 20, https://doi.org/10.1017/s1463423619000434.
[7] Valls, A., J. Piera and J. Tolra (n.d.), Report of in depth analysis of Badalona Healthcare services (BSA)” case study.
[23] Vallve, C. et al. (2016), SELFIE 2020: Work Package 2: Thick descriptions of the two Catalan case studies, Badalona Serveis Assistencials (BSA) (Spain).
[10] Vela, E. et al. (2018), “Population-based analysis of patients with COPD in Catalonia: a cohort study with implications for clinical management”, BMJ Open, Vol. 8/3, p. e017283, https://doi.org/10.1136/bmjopen-2017-017283.
[16] Vis, C. et al. (2015), “Implementing and up-scaling evidence-based eMental health in Europe: The study protocol for the MasterMind project”, Internet Interventions, Vol. 2/4, pp. 399-409, https://doi.org/10.1016/j.invent.2015.10.002.
[30] WHO (2018), Primary Health Care (PHC) Expenditure as % Current Health Expenditure (CHE).
Note
← 1. A “new model of primary care” meeting the following four characteristics: 1) multidisciplinary practices or inter-professional practices; 2) comprehensive health services in the community; 3) population health management (generally based on risk stratification using sophisticated IT systems); and 4) engagement of patients in shared decision-making (OECD, 2020[27]).
