People today are living longer with complex health needs. This has prompted countries to implement patient-centred, integrated models of care. Chapter 1 outlines key findings and policy recommendations to promote integrated care based on a review of strategically important care models operating in OECD and EU27 countries.
Integrating Care to Prevent and Manage Chronic Diseases

1. Key findings and recommendations
Abstract
Key messages
In OECD countries, two in three people aged 65 years and over live with at least one chronic condition. People living with chronic conditions often require care from different providers in multiple healthcare settings. To meet the needs of these people, countries are transitioning towards patient-centred, integrated models of care. As highlighted by the COVID‑19 pandemic, such models of care play a key role in making health systems more resilient.
This document outlines findings and policy recommendations following a review of 13 integrated care case studies selected in consultation with country delegates. Findings and recommendations cover the key dimensions of integrated care – governance, financing (payment models), digital tools and health information systems, and the workforce – as well as monitoring and evaluation, health equality, and scaling-up and transferability. Addressing the key dimensions of integrated care ultimately places the patient at the centre of their care thereby improving patient experiences and outcomes.
Governance
Governance structures covering health and social care sectors are often fragmented, which hinders the implementation of population-wide integrated care models. Findings from selected case studies highlight the importance of strengthening governance structures by breaking down silos across administrative systems in health and social care with the support of key stakeholders. For example, the Badalona City Council in Spain merged health and social care services into one integrated health and social care organisation called Badalona Serveis Assistencials (BSA). BSA’s governance model brings together all stakeholders, crucially policy leaders, which has created a strong commitment to, and culture of, integrated care.
Financing (payment models)
Traditional payment models, such as fee‑for-service, pay providers for the activities they perform. Such models do not promote care integration and may contribute to excessive expenditure. Countries can consider other innovative payment models that encourage providers to deliver co‑ordinated care. These include add-on payments to employ a case manager; episode‑based bundled payments, whereby providers receive one comprehensive payment per patient along a clinical care pathway; or comprehensive capitation payment models that cover a set of providers for a specific population. The OptiMedis integrated care model operating in certain regions of Germany, for example, utilises a comprehensive capitation payment model with a shared savings contract. This payment model incentivises provider networks to deliver high-quality care given they receive a proportion of the difference between expected and actual healthcare costs.
Workforce
Several barriers prevent health professionals from delivering patient-centred, multidisciplinary care, such as a culture of professional silos. Further, health professionals are not always supported to deliver integrated models of care. Actions to embed multidisciplinary care into everyday practice include investing in training programmes to teach health professionals new hard and soft skills, such as shared decision-making, inter-professional collaboration, and socio-cultural competencies. In addition, it is important to promote new professional roles that support care integration. For example, in the Basque Country, Spain, patients living with multimorbidities are assigned a case manager who works closely with a hospital liaison nurse to co‑ordinate care once the patient is discharged from hospital. Similarly, Poland has introduced care co‑ordinators as part of its strategy to enhance primary care.
Digital tools and health information systems
Digital tools play a key role in supporting integrated care. This is highlighted by selected case studies including Hospital-at-Home services in Catalonia, Spain, telehealth services for patients with chronic diseases in Italy, the Czech Republic, and Denmark, and an mHealth app for patients with asthma. However, the widespread use of digital tools is hindered by several factors including low levels of digital health literacy among patients and professionals.
Digital inclusion activities targeting vulnerable populations such as providing affordable and reliable broadband internet is one of several policies to increase uptake of digital tools among the population. For example, during the COVID‑19 pandemic, Technology Enabled Care in Scotland, which aims to scale‑up digital health programmes, provided over EUR 5 million to improve access to digital health services for vulnerable populations. For health professionals, uptake can be improved by implementing digital health competency frameworks to ensure they have the skills to utilise electronic health records and other eHealth tools. As an example, Finland created the national MEDigi project, which aims to harmonise and improve eHealth training for doctors and dentists.
Monitoring and evaluation
Evaluations of selected case studies focused on changes in patient experiences and healthcare utilisation. For example, the TeleCOPD (chronic obstructive pulmonary disease) programme operating in Southern Denmark recorded a drop in hospital admissions as well as a self-reported improvement in managing symptoms. Data on health outcomes and results from economic evaluations, however, were scarce among case studies. To build the evidence base supporting integrated care, there should be a focus on measuring structural, process and outcome indicators specific to integrated care that are comparable across countries. Example indicators include hospital readmissions, mortality after hospital discharge, prescription of appropriate medication for secondary care prevention, and use of digital tools. In addition, researchers should focus on undertaking economic evaluations that use robust methodologies to measure outcomes in relation to costs.
Health equality
Vulnerable populations are at greater risk of experiencing care fragmentation. Some actions were taken by selected case studies to narrow existing health inequalities. For example, by adapting programmes into languages spoken by minority groups, as was done for a patient-provider portal operating in the Finnish City of Oulu. Overall, however, tangible actions to adapt models of care to suit the needs of vulnerable populations were limited. To reduce existing health inequalities, future studies of integrated care models should examine the impact of integrated care models by stratifying data according to vulnerable populations with findings used to adapt care to better meet the needs of these patients. More broadly, investing in health literacy programmes that focus on vulnerable populations will help narrow existing health inequalities.
Scaling-up and transferrals
Only half of all selected case studies were explicitly scaled-up or transferred, however, nearly all were based on a pre‑existing model of care. Utilising existing frameworks to measure a region’s readiness to implement best practice integrated care models will facilitate their expansion. Example frameworks include the SCIROCCO (Scaling Integrated Care in Context) Maturity Model for Integrated Care as well as OECD’s Transferability Framework for public health interventions. Promoting close ties between owners and adopters of best practice models is also important for ensuring “lessons learnt” from past transfers are considered in the future. For example, administrators of ParkinsonNet, a Dutch programme for patients with Parkinson’s Disease, highlighted the importance of having a “champion” to drive the project. Similarly, administrators of Personalised Action Plans (PAPs) in Andalusia, Spain, noted several transfer facilitators including the importance of linking PAPs with patient electronic health records.
Introduction
A growing proportion of people in OECD and EU27 countries live with complex health needs. Stronger healthcare systems and better socio-economic conditions mean people today live longer: between 1970 and 2019, life expectancy (LE) among OECD and EU27 countries increased by over 11 years (OECD, 2021[1]). Concurrently, people lead increasingly unhealthy lifestyles characterised by poor diets and physical inactivity, and are more likely to suffer from poor mental health. As a result, a growing proportion of the population live with complex health needs and require care from different providers in multiple healthcare settings.
Better care co‑ordination is necessary to meet the changing health needs of the population. It is important that patients with complex health needs receive co‑ordinated care centred on their individual needs (see Chapter 2 for information on how integrated care promotes patient-centredness). OECD and EU27 countries have responded by implementing a number of patient-centred, integrated care models. These models aim to improve patient experiences and population health, reduce per capita costs of healthcare, create a better work/life balance among health professionals, and advance health equity.
The COVID‑19 pandemic highlighted the need to deliver patient-centred, integrated care. COVID‑19 led to a rapid surge in the number of acutely ill patients needing treatment. To maintain preventative care services as well as manage care for patients with chronic conditions, countries introduced policies that altered the delivery of care. For example, many OECD and EU27 countries relied on digital tools to deliver patient-centred, integrated care such as teleconsultations, ePrescriptions, and hospital-at-home services (OECD, forthcoming[2]).
Despite efforts to promote integrated care, co‑ordination among providers remains fragmented. As outlined within a 2020 OECD report on primary care, international data shows there continues to be “significant problems with the co‑ordination of care between primary healthcare teams, specialists, and hospitals” (OECD, 2020[3]; Barrenho et al., 2022[4]).
This report analyses a selection of strategically important integrated care models operating in OECD and EU27 countries using a validated performance assessment framework. Thirteen case studies were selected based on submissions from delegates to the OECD (see Table 1.1). For this reason, the report does not cover all models of integrated care, rather, it focuses on those that are of key strategic interest to policy makers. OECD’s Best Practice Identification Framework, which was co-created with member countries, formed the structure of the assessment (OECD, 2022[5]).
Findings and policy recommendations are grouped according to themes covering the key dimensions of integrated care. These themes are governance, financing (payment models), digital tools and health information systems, and the workforce (Wodchis et al., 2020[6]). In addition, the review covers monitoring and evaluation, health equality, and scaling-up and transferability, all of which are important for spreading best practices (OECD, 2022[5]). Findings and recommendations are based on a review of the 13 selected case studies. Therefore, this report does not comprehensively address all issues related to integrated care in all contexts, but rather offers interesting insights and highlights the value of applying a common assessment methodology.
Findings and recommendations from this report can help make health systems more resilient against future shocks. COVID‑19 had a profound impact on health systems across the world. Future shocks are inevitable. Therefore, it is important countries enhance the resilience of their healthcare system by promoting integrated care based on the policies outlined in this report.
Table 1.1. Overview of selected case study interventions
|
Name and description |
Country* |
|---|---|
|
OptiMedis, regionally based integrated care model The OptiMedis integrated care model emerged in 2005 following reforms in Germany to promote care co‑ordination. The model of care, which operates in the west (state of Hesse) and south-west region (state of Baden-Württemberg) of Germany, aims to improve patient experiences and population health, while reducing per capita costs. A key feature of the care model is its “shared savings contract”, which incentivises the delivery of high-quality, preventative care |
EU-supported Joint Action – JADECARE** |
|
Hospital-at-Home programme The Hospital-at-Home (H@H) programme offers patients acute, home‑based care that would otherwise be delivered in a hospital setting. |
JADECARE Catalonia, Spain |
|
Oulu’s Self Care Service Oulu’s Self Care Service (SCS) is a digital patient provider portal available to all residents. SCS offers patients a range of online primary care services such as online appointment booking and ePrescriptions. For health professionals, SCS provides guidelines and care pathways based on individual patient data. |
Finland |
|
Integrated care model for multimorbid patients As part of the strategy for chronicity in the Basque Country, Spain, an integrated care model was implemented that includes a comprehensive baseline assessment; individualised care plans; care from a multidisciplinary team; co‑ordinated hospital discharge; patient empowerment programmes; and a strong health information system. Eligible patients are identified through a sophisticated risk stratification system, which covers 100% of the population. |
Basque Country, Spain |
|
Badalona Healthcare Services The Badalona City Council developed an integrated care organisation bringing together health and social care sectors – Badalona Serveis Assistencials, BSA. In addition to organisational integration (i.e. combining health and social care), BSA creates other forms of integration such as professional integration with the use of multidisciplinary teams and normative integration by developing a shared organisational and professional culture. |
Badalona, Spain |
|
Medical Diagnostic Centre (MDC) MDC is a primary care model for patients with chronic conditions. Patients who access MDC obtain an Individual Medical Care Plan based on a comprehensive assessment by a general practitioner. Results from the comprehensive assessment are used to stratify patients into risk groups, which helps health professionals proactively manage patient needs. Following the comprehensive assessment, patients receive care from a multidisciplinary care team, which is co‑ordinated through a case manager. |
Poland |
|
TeleHomeCare TeleHomeCare is a digital intervention designed to support home care through telemonitoring and teleconsultation for patients who suffer from one or more of the following chronic diseases: heart failure, chronic obstructive pulmonary diseases, and diabetes. The programme operates in the Italian town of Ceglie Messapica. |
Italy |
|
Digital Roadmaps towards an integrated healthcare system The Digital Roadmap initiative aims to improve co‑ordination across healthcare settings and therefore care for patients, with a specific focus on those living with one or multiple chronic conditions. The initiative comprises several digital care interventions such as TeleCOPD, Telepsychiatry, virtual rehabilitation services and an mHealth app. |
Southern Denmark |
|
Technology Enabled Care (TEC) The TEC programme in Scotland is to ensure that successful digital health and care initiatives are mainstreamed. At the national level TEC provides leadership, evidence, and guidance on mainstreaming TEC to the government, healthcare providers and other stakeholders. It also invests in national infrastructure, such as national licenses for digital care tools. At a local level, it helps to grow TEC initiatives by providing dedicated funding, as well as change management support and knowledge exchange, to organisations implementing or trialling such initiatives |
Scotland |
|
Telemonitoring for patients with advanced heart failure The University Hospital Olomouc in the Czech Republic implemented a telemonitoring intervention for patients with advanced heart failure. As part of the intervention, a patient’s vital signs are automatically shared daily with health professionals at the hospital including blood pressure, blood saturation, and results from electrocardiograms. |
Czech Republic |
|
ParkinsonNet ParkinsonNet was developed to deliver high-quality, specialist care for Parkinson’s disease. Through regional networks, allied health interventions are delivered by specially trained therapists who work according to evidence‑based guidelines. |
Netherlands |
|
Personalised Action Plans (PAPs) Andalusia, Spain, introduced PAPs for people living with one or more chronic diseases. The PAP programme outlines a formal process whereby practitioners and patients collaborate to create a longitudinal treatment plan. |
Andalusia, Spain |
|
Mobile Airways Sentinel Network (MASK) MASK is an mHealth intervention designed to reduce the burden of allergic rhinitis (AR) and asthma. MASK is broken into two components – one for individuals and the other for health professionals. Individuals can download the MASK-air app for free which includes an allergy diary. Health professionals have access to a MASK-air Companion, an electric decision support system to promote personalised treatment for patients with AR and asthma |
Several OECD and EU‑27 countries |
Note: *The case study may operate across the country or in specific regions within that country. **Joint Action on implementation of digitally enabled integrated person-centred care.
Governance and financing
Traditional governance structures and payment models prevent widespread care integration
Many case studies pursued care integration at a specific level of care, such as primary care, and often for a specific disease. For example, the Finnish City of Oulu implemented a digital patient-provider portal at the primary care level, while programmes such as ParkinsonNet in the Netherlands cater to the needs of patients with Parkinson’s disease. Only a small number of case studies operate across the entire spectrum of healthcare services for whole populations, such as the OptiMedis model in certain regions of Germany and Badalona’s (Spain) integrated care organisation.
The limited number of integrated care models covering entire populations and all healthcare services is in large part due to existing governance structures. Governance systems across and within health and social care sectors are often fragmented making it difficult for providers to work together to deliver patient-centred, integrated care. For example, in some countries, primary care is governed at the national level while inpatient care falls under the responsibility of regions, which hinders vertical care integration. Further, in countries with social health insurance or private compulsory insurance, long-term care isn’t necessarily included in the scope of insurance and is therefore governed and financed separately (Barrenho, Fujisawa and Kendir, 2020[7]).
Traditional payment models can also discourage care integration. Specifically, in most OECD countries, providers are paid for the activities they perform – i.e. using fee‑for-service (FFS) or diagnostic-related groups (DRGs). The former pays providers based on the service provided, while the latter pays providers for every patient treated. Both FFS and DRGs contribute to care fragmentation and excessive health expenditure (Lorenzoni and Milstein, 2022[8]). For example, in Badalona, Spain, despite integrating health and social care into one organisation, different types of care are financed separately – e.g. primary care is financed based on the population covered, which is adjusted for several factors such as age, while hospitals are paid for each service provided. The variability of financing methods “hinders the management of services, which are thought from an integrated perspective but financed from different budgets” (Vallve et al., 2016[9]) (see Chapter 7). Changes in financial payment models can have a significant impact on the way care is delivered, but ultimately are only a means, not an end, for integrating care.
Policy recommendations
Embed integrated care within the health system’s governance structure
Stronger governance systems that facilitate care integration across and within health and social care sectors are necessary for deploying population-wide integrated care models covering all services. How countries achieve this is complex and context-specific. For this reason, this high-level report on integrated care does not seek to map out the multiple paths to achieve strong governance systems that support care integration. Instead, it acknowledges the importance of strengthening governance structures by breaking down silos across administrative systems in health and social care with the support of key stakeholders.
Among selected case studies, an integrated care model in the Basque Country, Spain, highlights how countries can strengthen governance structures to promote better care for multimorbid patients. At a high level, the region introduced integrated health organisations to replace independently run hospitals, primary and outpatient care centres (see Chapter 6). Similar changes were introduced in 2000 in the Spanish municipality of Badalona (see Chapter 7). See Box 1.1 for further details.
Box 1.1. Case studies: Integrated health organisations
Strong governance structures promote integrated care. Example policies implemented to strengthen governance structures among selected case studies are detailed below.
Integrated Health Organisations, the Basque Country, Spain
In response to challenges posed by multimorbidity, in 2010 the Basque Country’s Department of Health launched the “Strategy to tackle the challenges of chronicity” (Ministry of Health and Consumer Affairs, 2010[10]). The objective of the strategy was to “re‑orient the health system toward an integrated care model” that is patient-centred and meets the needs of people with chronic conditions (The CareWell Group, 2018[11]).
To realise this objective, the Basque Country transformed from a system made up of 35 independent organisations (15 hospitals and 20 primary healthcare centres, as well as an additional 475 outpatient health centres) to one comprising 13 integrated health organisations (IHOs), a well as two hospitals and three mental health networks. Each IHO is set up around a regional hospital and offers a range of services for a geographically defined population (Izagirre-Olaizola, Hernando-Saratxaga and Aguirre-García, 2021[12]).
Providers within an IHO have the same management and objectives, further, each IHO has its own budget. A single budget for an IHO is designed to encourage providers to work together to ensure services are provided at the right level of care (Izagirre-Olaizola, Hernando-Saratxaga and Aguirre-García, 2021[12]).
Changes to the governance structure and the delivery of healthcare (i.e. by multidisciplinary care teams) contributed to an improvement in access to primary care and reduced demand for inpatient care. Further, patients and carers who participated in the integrated care model provided largely positive feedback – for example, health professionals felt more alert and watchful, while patients felt they received more co‑ordinated care and that the management of information improved (Mateo-Abad et al., 2020[13]).
Badalona Healthcare Services, Badalona, Spain
Before 2000, health and social care services operated in silos within Badalona. Specifically, the Badalona Healthcare Services (Badalona Serveis Assistencials, BSA) was responsible for healthcare while the City Council operated social services. This arrangement led to service duplication and uncoordinated care delivery. In response, in 2000, the Badalona City Council agreed to merge health and social care services into one integrated health and social care organisation. This organisation goes by the name of BSA and is owned by the Badalona City Council.
BSA’s governance structure supports several types of care integration within the health and social care system, for example, functional integration (back-of-office and support function co‑ordination), organisational integration (single organisation responsible for health and social care services), and professional integration (multidisciplinary care teams including primary care doctors, specialists, doctors, and nurses based in hospitals, and social workers).
Benefits generated by BSA include better adherence to treatment due to clinical pathways, improved co‑ordination between different levels of care and with third-party providers and improved organisational and decision-making processes.
Consider innovative payment models that incentivise care integration, while recognising that the current evidence on their impact is mixed
Payment models play a key role in incentivising providers to deliver high-quality, integrated care that is affordable. Three payment models of particular interest are 1) add-on payments; 2) episode‑based (bundled) payments; and 3) comprehensive capitation payments.
Countries can consider these innovative payment models to promote integrated care delivery. However, it is noted that real-world evidence supporting these models of payment is mixed, ranging from no changes to standard delivery of care, or higher expenditures without quality improvements, to improved quality and lower health expenditures.
Add-on payments: Add-on payments refer to additional payments made on top of existing payment models to incentivise desired behaviours, including integrated care. Among OECD countries, 12 use this payment model to incentivise prevention or co‑ordination: Australia, Austria, Canada, Denmark, France, Germany, Iceland, Israel, Italy, Mexico, Norway,1 and Sweden (OECD, 2018[14]). Add-on payments to incentivise integrated care may be referred to as pay-for-co‑ordination (P4C). For example, an additional payment to primary care providers for undertaking a comprehensive review of a patient’s case involving notes from several providers, or a payment to employ a case manager (Struckmann et al., 2016[15]). Add-on payments typically target individual providers, usually physicians, and do not change the base structure of existing payment models. Therefore, add-on payments can be introduced more easily than bundled or comprehensive capitation payment models.
Episode‑based (bundled) payments: Episode‑based payment models bundle the activities of different providers, such as a hospital and an outpatient physician, along one care pathway (Lorenzoni and Milstein, 2022[8]; Lindner and Lorenzoni, forthcoming[16]). Providers then receive one comprehensive payment per patient for the clinical care pathway. Several OECD member countries have introduced episode‑based payments for chronic conditions (e.g. the Netherlands and the United States) or for surgical interventions (e.g. France and Norway). For the former, providers receive a budget covering all condition-related services within a given period, while for the latter, a group of providers receive a joint price per patient treated (Lorenzoni and Milstein, 2022[8]; Lindner and Lorenzoni, forthcoming[16]).
Comprehensive capitation payments:2 comprehensive capitation payment models cover the activities of a set of providers that provide care over a given period. Under this model, a network of providers generally receives a yearly or monthly joint payment for every patient covered in a programme (Lorenzoni and Milstein, 2022[8]; Lindner and Lorenzoni, forthcoming[16]). The payment per patient is typically adjusted for age, sex, and health status to account for differences in costs. The payment may also include quality-related adjustments to further incentivise the provision of high-quality care. The OptiMedis model in Chapter 3 utilises a comprehensive capitation payment model with a shared savings contract, as summarised in Box 1.2. Under this model of care, provider networks are incentivised to deliver integrated care given they receive any realised healthcare expenditure savings. Comprehensive capitation payments are typically harder to implement given they require stronger governance arrangements, as well as improvements in data collection, analysis, monitoring, and reporting. Therefore, it is not surprising that only three OECD countries have implemented such payment models (i.e. France, Germany and the United States).
Box 1.2. Case study: The OptiMedis model of care – comprehensive capitation payment model with a shared savings contract
The OptiMedis model involves the creation of a regional integrator, an institution in charge of managing the network integration with a physical presence in the region and legally constituted as an enterprise. Healthcare providers in partnership with the network participate in the regional integrator in the capacity of partners, owners, or associates (depending on the context) together with OptiMedis AG, a German healthcare management company with an expertise in management support, business intelligence and health data analytics.
A key feature of the OptiMedis model is the payment system, which is based on a “shared savings contract”. The contract is drawn between the integrated network on one side and sickness funds on the other. As part of this contract, positive differences between expected costs* and the real healthcare costs of the population the network is accountable for are considered “savings” and are shared between the integrated network and sickness funds.
The share of savings received by the integrated network is used to finance integration efforts, including performance bonuses and operations of the regional integrator. Any remaining profits are re‑invested in the regional healthcare system.
To avoid an under provision of services to generate savings, there are minimum quality standards that need to be complied with. The payment system is therefore designed so that there is a financial incentive to invest in delivering high-quality, efficient, preventative care.
Using OECD’s Strategic Planning for Public Health microsimulation model and real-world data from OptiMedis, this model of care is estimated to lead to an additional 146 441 life years and 97 558 disability-adjusted life years by 2050 in Germany. Over the same period, cumulative health expenditure savings per person are estimated at EUR 3 470 in Germany.
Note: *Expected costs are calculated according to the risk-adjusted funds received by the sickness funds to care for their contracted insurees from the central authority (Gesundheitsfonds).
Workforce
Barriers such as a culture of professional siloes and systems not suitable for sharing patient data prevent health professionals from delivering patient-centred, multidisciplinary care
Patients with complex health needs access care from several health professionals. For example, a patient with type 2 diabetes and hypertension may require care from a general practitioner (GP), a dietician, a cardiologist, and a practice nurse. To ensure treatment is co‑ordinated and patient-centred, these patients should receive care from a multidisciplinary care team (see Box 1.3). For example, evidence‑based clinical guidelines are often disease‑specific and do not consider the cumulative impact of different treatments (Hughes, McMurdo and Guthrie, 2012[17]). Therefore, it is important that a team of professionals, along with the patient or carer, develop individualised care plans based on factors such as interactions and the level of burden placed on the patient.
Box 1.3. Multidisciplinary care teams
Multidisciplinary care teams include two or more health/social/community professionals who work together to provide comprehensive care centred on the patient’s needs. Chosen professionals may function under one organisation or come together from different organisations.
Professionals who make up the multidisciplinary care team will depend on the needs of the patient. Examples of professionals include:
General practitioners (GP)
Medical specialists
Practice nurses
Community health nurses
Allied health professionals (e.g. dieticians, psychologists, pharmacists, occupational therapists)
Social workers
Health educators
Long-term care manager
Geriatricians.
Multidisciplinary care teams specify a case manager. The case manager has many roles including maintaining team co‑ordination, managing a patient’s treatment schedule, tracking patient progress, making referrals, as well as communicating the patient’s health status to the team (Saint-Pierre, Herskovic and Sepúlveda, 2017[18]). Evidence from the literature indicates that “well-organised” multidisciplinary care teams improve patient satisfaction and reduce staff burnout (Leach et al., 2017[19]).
For real-world examples, see case studies from the Basque country, Spain (Chapter 6), and Poland’s medical diagnostic centres (Chapter 8).
Barriers to implementing patient-centred, multidisciplinary care include, but are not limited to, a culture of professional silos, lack of resources, national or regional legislation that restricts providers from sharing patient information, lack of financial incentives to encourage professionals to work together, and undefined relationships across professionals. Furthermore, professionals often do not have the skills to work as a team given they receive their training and work experience in different settings (e.g. one in four general practitioners work in private solo practices, see Figure 1.1) (OECD, 2020[3]). Difficulties transitioning to multidisciplinary care occurred in Badalona, Spain, which saw “resistance and conflict among professionals”. Specifically, social care workers did not support their portfolio of services being managed by an enterprise from the health sector, while medical staff resisted the introduction of domiciliary services (Vallve et al., 2016[9]) (see Chapter 7 for more details).
Figure 1.1. One in four general practitioners work in solo practices
Where are primary care services predominantly provided?
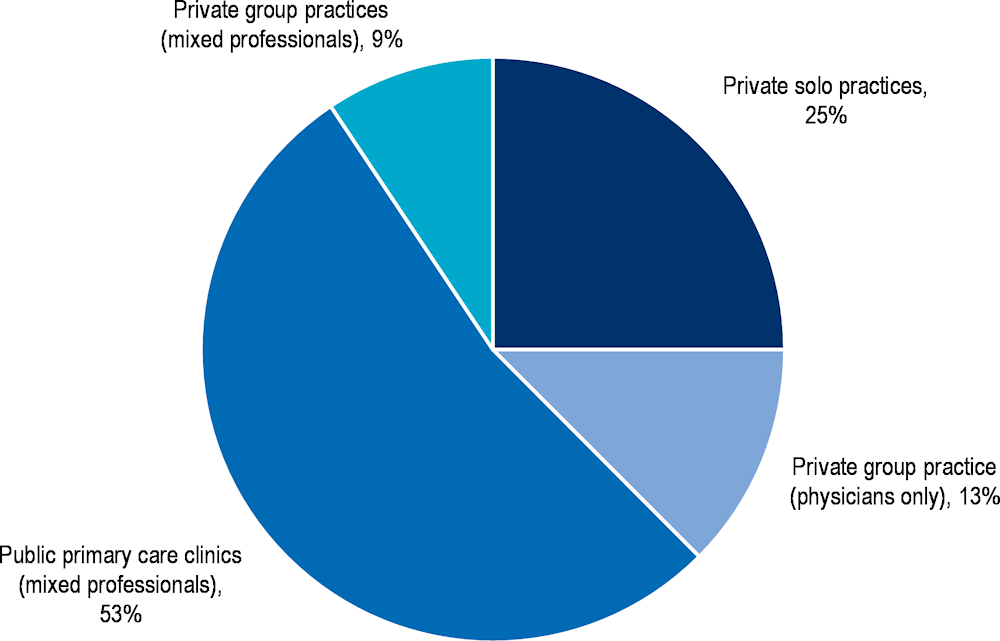
Note: Data collected from 32 OECD countries.
Source: OECD (2016[20]), “Health Systems Characteristics Survey 2016”, https://qdd.oecd.org/subject.aspx?Subject=hsc.
Despite playing a lead role in delivering integrated care, the primary care workforce is not always sufficiently supported to take on new roles
Primary healthcare workers are often the first point of contact for people accessing the healthcare system. This includes people with minor ailments to those with complex health needs. Therefore, primary healthcare professionals play a key role in providing co‑ordinated, patient-centred care from the earliest possible point in time. Despite growing consensus that a strong primary healthcare sector is essential for an effective, efficient, and equitable healthcare system, countries often prioritise secondary and tertiary care (Hanson et al., 2022[21]).
From selected case studies, there is some evidence that primary care staff are not sufficiently supported. For example, a review of the Basque Country’s integrated care model found primary care professionals felt their workload markedly increased, particularly among nurses who were now responsible for leading weekly education sessions and following-up with patients more regularly (Mateo-Abad et al., 2020[13]). See Chapter 6 for further details.
Policy recommendations
Invest in training programmes to upskill the health workforce
The workforce requires appropriate skills to deliver patient-centred, integrated care to those with complex health needs. Health systems must therefore invest in training programmes that teach health workers vital “hard” and “soft” skills:
Hard skills: New ways of work require health professionals to develop new technical skills. Building digital health literacy among the health workforce is of particular importance given ICT tools play a key role in promoting care integration (e.g. electronic health records and patient provider portals). See the section on “Digital tools and health information systems” for further details.
Soft skills (or transversal skills): The transition towards patient-centred, multidisciplinary care represents a major cultural shift for many health professionals. To adjust to this new way of work, health professionals must acquire new soft skills (i.e. non-technical skills). These include shared behavioural counselling, communication, collaboration, and relationship building (Ranjan, 2015[22]). For example, in Badalona, Spain, health professionals highlighted the importance of those providing care in a patient’s home to have specific skills related to “flexibility, teamwork, communication, and empathy” (Vallve et al., 2016[9]).
Introducing training programmes into the formal curriculum can ensure all health professionals obtain the same skills thereby promoting multidisciplinary care. It is possible to supplement formal training (i.e. continuing medical education) with informal training by establishing “learning networks”. Learning networks led by health professionals can help spread good practices, for example, through webinars, conferences, as well as online materials and guidebooks.
Promote new professional roles that support integrated care, such as case managers
Integrated care requires the establishment of new professional roles, in particular case managers (Looman et al., 2021[23]). Case managers are responsible for co‑ordinating professionals, the patient and their carer (see Box 1.3). Case managers represent a relatively new professional role; therefore, it is important that:
Case managers have a well-defined role: there needs to be clarity on their role and that this is well understood among the multidisciplinary care team, patient, and carer.
Case managers have the right skills: an effective case manager has many skills that extend beyond clinical knowledge. These include interpersonal skills, problem-solving skills, and negotiation and brokerage skills.
Among selected case studies, case managers were typically nurses, however, they may also come from other qualified backgrounds such as social and community workers. For example, case management within Badalona’s integrated care organisation in Spain is led by both nurses and social workers (see Chapter 7). Another example comes from Austria, which, as part of its Recovery and Resilience Plan, will implement “Project Community Nursing” to promote the role of community nurses in delivering integrated care (Box 1.4).
In the right context, assigning case manager roles to community or social workers can result in several benefits. These include (Kim et al., 2016[24]; Berini, Bonilha and Simpson, 2021[25]; Kim et al., 2016[26]; OECD, 2020[3]):
An improvement in patient satisfaction and health outcomes
Reduced pressure on primary care nurses and doctors
A reduction in healthcare costs
A reduction in health inequalities.
Box 1.4. Project Community Nursing – Austria
Funded by the EU (NextGenerationEU), Austria will implement Project Community Nursing as part of its Recovery and Resilience Plan, in which community nurses will take on various roles to promote care integration including:
Providing low-threshold support and relief services close to the patient’s home
Networking between patients and care providers
Co‑ordinating care services for patients, covering both health and social care services
Undertaking health prevention and promotion activities, such as building health literacy.
Community nurses will focus on caring for vulnerable populations, namely older people living at home and their relatives. However, the target group may expand to meet the specific needs of the local community.
Over 100 pilots will be deployed as part of Project Community Nursing across Austria. A level of homogeneity is guaranteed across the pilots given they are co‑ordinated at the national level.
Assigning community workers as case managers is particularly beneficial when treating vulnerable and hard to reach patients such as racial and ethnic minorities, as well as those with a low socio-economic status and/or living in a rural area. For example, a community worker with a close understanding of the population being served can act as a liaison between health, social and community services thereby facilitating access to culturally appropriate care (American Public Health Association, 2022[27]). For the reasons outlined above, health systems should develop their community health workforce and ensure they can take on new roles, including case management.
Case managers are not the only new professional role to emerge from the transition to integrated care. New professional roles identified among selected case studies include:
Referent internist who supports decisions made at the primary care level as well as co‑ordinating specialists involved in treating the patient in the hospital
Hospital liaison nurse who works with a primary care nurse (who is also the case manager) to co‑ordinate care when the patient is discharged from the hospital
Domiciliary attention physician who provides care to patients either in the hospital or in a home setting.
Digital tools and health information systems
Digital tools support patient-centred, integrated care by improving the flow of information between providers and patients
Digital tools enable integrated care by improving communication and co‑ordination across service providers, for example, between hospitals and home‑ and community-based care as well as transitions between health and social care. Digital tools also enable communication channels between patients and providers, thereby promoting patient-centredness (OECD, 2019[28]).
Digital tools included within selected case studies can be categorised into one of three groups: eHealth, big data and mHealth (Fahy and Williams, 2021[29]). The role each of these technologies plays in promoting integrated care is summarised below, with real-world examples from selected case studies available in Box 1.5:
eHealth uses information and communication (ICT) technologies to improve communication processes and ways of recording patient information. Example technologies include electronic health records (EHRs), patient portals and telehealth.
Big data collected from sources such as EHRs can be used to stratify the population into different risk categories, which helps deploy population-based integrated care models. Big data also supports population monitoring, research, innovation, and continuous improvement of health system effectiveness.
mHealth offers people access to new services using mobile phone devices and apps. These services aim to empower people and encourage healthy lifestyle behaviours, improve communication between patients and providers, and may also provide important diagnostic and treatment information.
Box 1.5. Case studies: Digital tools to promote integrated care
This box summarises digital tools identified in selected case studies to promote integrated care.
Patient portals
Patient portals give people access to their health data in an easy-to‑understand format. Finland’s City of Oulu has deployed a voluntary digital patient-provider portal focused on primary care and to a lesser extent social care. With the patient’s consent, data from a patient’s EHR is uploaded to the portal ensuring primary care professionals have access to patient data. The portal allows patients to book appointments, communicate with health and social care professionals on non-urgent matters, share home monitoring test results (e.g. blood pressure), and access information on health prevention. For providers, the portal provides tailored guidelines and care pathways based on individual patient information such as laboratory results.
Big data
In line with the strategy for chronicity, the Basque Health Service, Spain, developed an integrated care model for multimorbid patients. The model has several key characteristics including individualised care plans, care delivery by a multidisciplinary team and patient empowerment programmes. Patients eligible for this model of care are identified using a sophisticated risk stratification system – i.e. Johns Hopkins Adjusted Clinical Groups Predictive Model (ACG-PM). ACG-PM uses patient data to predict utilisation of healthcare services (a proxy measure for patient morbidity) over the next 12 months.
mHealth apps
mHealth apps improve communication between patients and providers, while simultaneously encouraging patients to take control of their own health. Chapter 15 includes a description of the Mobile Airways Sentinel Network (MASK) mHealth app, which helps reduce the burden associated with allergic rhinitis (AR) and asthma. The mHealth app has two components, one for individuals and another for health professionals:
For patients: users are encouraged to upload daily data related to topics such as allergy symptoms and treatment. Including data from a patient’s EHR to complement self-reported information is possible.
For health professionals: physicians and pharmacists have access to the MASK-air Companion, which is interoperable with the patient app. The Companion is an electronic decision support system to assist health professionals diagnose and provide personalised treatment to patients.
MHealth apps were explored in previous work by OECD on best practices in public health. Specifically, the best practice booklet on healthy eating and active lifestyles examined the web- and mobile‑based intervention, “Let Food Be Your Medicine”, which provides users with personalised nutrition advice (OECD, 2022[30]).
Utilisation of digital health tools is lower among vulnerable populations
OECD populations are increasingly reliant on the internet to access information and services, including in the health sector. For example, between 2007 and 2021 the proportion of adults seeking health information online in the last three months increased by over 150% (i.e. from 25% to 62%) (OECD, 2019[31]). Nation-wide averages on the use of digital health tools, however, mask stark differences across population groups. Specifically, vulnerable populations including the elderly, racial and ethnic minorities, and those with a lower socio-economic status and/or living in a remote area are less likely to: a) be digitally literate and b) have access to the internet as well as smartphone devices. For these reasons, digital tools risk exacerbating existing health inequalities as highlighted by selected case studies:
Age inequalities: health professionals involved in the integrated care model operating in the Basque Country, Spain, highlighted that digital tools within the model of care (e.g. Personal Health Folders, which allow patients access to their information) hold great promise, but are limited given older patients lack the necessary technical skills.
Geographical inequalities: administrators of TeleHomeCare, as implemented in the Italian city of Ceglie Messapica for multimorbid patients, identified technical difficulties implementing TeleHomeCare in areas where there was poor or no internet network coverage.
Digital tools are not widely used among health professionals
Several factors prevent health professionals from supporting digital health technologies. These include:
Low levels of digital health literacy with up to 70% of health workers stating they do not feel accustomed to using digital solutions “due to gaps in knowledge and skills in data analytics” (OECD, 2019[28]).
Additional burden posed by the digital tool due to insufficient training and/or poor design, which do not consider the needs of end users.
Distrust that the digital tool improves service delivery and therefore patient outcomes.
Digital tools to support integrated care are often deployed as small-scale pilots
Many case studies selected for this review include digital tools implemented locally, and often for a specific disease. Therefore, the selected case studies only covered a small number of eligible patients, which limited their overall impact. For example:
TeleHomeCare for certain chronic conditions in the Italian town of Ceglie Messapica only covered 207 patients (see Chapter 9)
Telemonitoring for patients with advanced heart failure has been implemented in just one hospital in the Czech Republic, which covers between 100 and 250 eligible patients (see Chapter 12).
This key finding aligns with previous OECD work on digital health, which states that innovative ways of delivering healthcare and supportive ICT are typically deployed as pilots or research projects, with project-specific funding (OECD, 2019[28]). Further, many digital tools are not scaled to reach a larger population even if they are successful or show promise (OECD, 2019[28]). There are several reasons for this such as issues with reimbursement mechanisms, interoperability and ICT infrastructure, culture of change and adoption of new technologies, and suitability of skills among staff (Oliveira Hashiguchi, 2020[32]).
Policy recommendations
Invest in digital inclusion activities targeting vulnerable populations
Digital inclusion activities ensure all individuals and communities, including the most vulnerable, have access to and use ICTs (National Digital Inclusion Alliance, 2022[33]). Specific activities to promote digital inclusion include:
Digital literacy training
Affordable and reliable broadband internet services
Internet-enabled devices that incorporate feedback from end-users, including patients
High-quality technical support
Applications and online content designed to enable and encourage self-sufficient, participation and collaboration
Offering incentives for and improving access to adult learning activities.
Efforts to promote digital inclusion among selected cases studies include Scotland’s Technology Enabled Care (TEC) programme, which, during the COVID‑19 pandemic created the “Connecting Scotland” initiative. As part of this initiative, TEC invested GBP 5 million (EUR 5.73 million) to provide internet connection, training and support, and a laptop or tablet to 9 000 people who were considered at clinically high risk. Further, as part of its latest strategic plan, TEC will offer support and funding to ensure care homes have reliable internet connections, devices and other infrastructure needed for digital care. It will also support the development and adoption of a suite of tools that can be used in care homes, such as telecare, video-consultations, messaging, and assessment tools.
Invest in activities that promote the use of digital tools among health professionals
This review identified several activities needed to promote the widespread use of digital health technologies among health professionals, namely:
Developing formal digital health literacy training by implementing digital health competency frameworks. For example, every university in Finland plans to provide medical students with streamlined digital health education – MEDigi – to ensure all doctors have appropriate digital skills. Curricula related to digital health should be frequently revised to reflect ongoing technological changes.
Providing additional training specific to the digital tool. For example, health professionals in the Finnish City of Oulu receive two‑hour training sessions on how to use the patient-provider portal, Self Care Service (SCS). Further, as part of TeleHomeCare in the Italian city of Ceglie Messapica, GPs and specialists receive two weeks’ worth of training run by control room operators and telemedicine experts. (See Chapters 5 and 9 for further details).
Involving health professionals in the design of digital tools to ensure technologies are integrated into current workflows, are non-burdensome, and are interoperable with patients.
Ensuring digital tools align with current practices to ensure they do not create additional work for health professionals.
Undertaking robust evaluations of digital health technologies to promote trust (discussed further under the section on “Monitoring and evaluation”). Given evidence is rapidly evolving in this space, there must be a supportive environment for knowledge accumulation and up-to-date evidence (e.g. publication of regular rapid reviews).
Institutional and organisational changes are needed to digitally transform the health sector
This review looked at a small selection of integrated care models, most of which are confined to a specific region within a country and in some cases are just pilots. Therefore, this review did not explore in detail the wider digital health system in which these models operate. Nevertheless, it is recognised that population-wide integrated care requires digitally advanced health systems.
Previous work by the OECD identified three main government actions to digitally transform health systems (OECD, 2019[28]). These are:
An overarching digital strategy that is comprehensive and includes a consolidated vision, plan, and policy framework.
Strengthening the governance of health data to enable data and digital technologies to be put to productive use while ensuring security and respect for individuals. At present, legal issues, a lack of trust among stakeholders, and non-unified data standards and exchange formats act as barriers to realising the potential of health data to improve outcomes.
Building institutional and operational capacity including preparing the workforce to harness opportunities presented by digital technology, as well as empowering the population. In addition, institutional systems must be in place to link, share and analyse patient data.3 This last point is of key importance given data fragmentation, weak data-sharing practices and a lack of interoperability between systems are some of the key barriers to providing integrated care.
Monitoring and evaluation
Evaluations of integrated care models focus on patient experiences and healthcare utilisation
Across the 13 selected case studies, less than half collected data on objective health outcomes such as changes in mortality. Selected case studies instead focused on measuring changes in patient experiences and utilisation of healthcare services (see Table 1.2). Further, two of the selected cases studies provided no evidence at all.
Table 1.2. Evidence measuring effectiveness by selected case studies
|
Measured changes in objective health outcomes |
Measured changes in subjective health outcomes (i.e. patient experiences) |
Measured changes in utilisation of healthcare services |
No evidence |
|
|---|---|---|---|---|
|
OptiMedis, regionally based integrated care model |
✓ |
✓ |
✓ |
|
|
Hospital-at-Home |
✓ |
✓ |
||
|
Mobile Airways Sentinel Network (MASK) app |
✓ |
✓ |
||
|
Oulu Self Care Service (patient portal) |
✓ |
|||
|
Integrated care model for multimorbidity, Basque Country |
✓ |
✓ |
✓ |
|
|
Badalona Healthcare Services (BSA) |
✓ |
✓ |
||
|
Medical Diagnostic Centre |
✓ |
✓ |
||
|
TeleHomeCare in the Italian city of Ceglie Messapica |
✓ |
|||
|
Digital Roadmaps towards an integrated healthcare system |
✓ |
✓ |
||
|
Technology Enabled Care (TEC)* |
✓ |
✓ |
||
|
Telemonitoring for patients with advanced heart failure |
✓ |
|||
|
ParkinsonNet |
✓ |
✓ |
✓ |
|
|
Personalised Actions Plans |
✓ |
✓ |
Note: *This report evaluated TEC as opposed to the individual interventions within TEC. An evaluation of each programme funded by TEC fell outside the scope of this review, therefore, it is possible that individual TEC funded programmes collected data on objective health outcomes.
The finding above aligns with the broader literature whereby (Baxter et al., 2018[34]):
Evidence supporting integrated care is strongest regarding patient satisfaction, perceived quality of care and access to care
Objective quality of care outcome measures is limited.
Integrated care models have the potential to deliver healthcare more efficiently, however, real-world evidence is limited
Efficiency refers to how well the mix of monetary and non-monetary inputs were used to achieve desired outcomes in a real-world setting (OECD, 2022[5]). In the health sector, economic evaluations such as cost-benefit or cost-effectiveness analyses are frequently used to measure efficiency.
Among selected case studies, none included results from an economic evaluation. Instead, many case studies relied on estimates measuring changes in health expenditure to prove efficiency (see Table 1.3). These estimates fail to show the whole picture given cost savings should be measured in relation to changes in outcomes. For example, an integrated care model may increase expenditure but still be efficient if changes in health outcomes are large.
Table 1.3. Evidence measuring efficiency by selected case studies
|
Economic evaluation |
Changes in health expenditure |
No evidence |
|
|---|---|---|---|
|
OptiMedis, regionally based integrated care model* |
✓ |
||
|
Hospital-at-Home |
✓ |
||
|
Mobile Airways Sentinel Network (MASK) app |
✓ |
||
|
Oulu Self Care Service (patient portal) |
✓ |
||
|
Integrated care model for multimorbidity, Basque Country |
✓ |
||
|
Badalona Healthcare Services (BSA)* |
✓ |
||
|
Medical Diagnostic Centre |
✓ |
||
|
TeleHomeCare in the Italian city of Ceglie Messapica |
✓ |
||
|
Digital Roadmaps towards an integrated healthcare system** |
✓ |
||
|
Technology Enabled Care (TEC)** |
✓ |
||
|
Telemonitoring for patients with advanced heart failure |
✓ |
||
|
ParkinsonNet |
✓ |
||
|
Personalised Actions Plans |
✓ |
Note: *Individual programmes within OptiMedis and BSA have results from an economic evaluation, but not the model as a whole. **Digital Roadmaps and TEC are both programmes that support a range of individual integrated care digital projects. Individual projects may have data on cost-effectiveness and/or changes in costs. Nevertheless, there is no data for the programmes as a whole.
The lack of robust data measuring the efficiency of selected case studies aligns with the broader literature. For example, a 2020 systematic review and meta‑analysis of integrated care models concluded there is a paucity of studies measuring cost-effectiveness and studies are not of high quality (Rocks et al., 2020[35]). Further, the 2021 Handbook on Integrated Care noted that the “substantial resources” necessary for collecting high-quality data pose a significant barrier to undertaking cost-effectiveness analyses (Tsiachristas and Rutten-van Mölken, 2021[36]).
Policy recommendations
Focus on developing and measuring indicators specific to integrated care
To understand the true impact of integrated care models, it is important to develop and measure indicators specific to the model of care under evaluation. Drawing upon the Donabedian approach to evaluating care quality, indicators should cover structures, processes and outcomes (Donabedian, 1988[37]; Report by the Expert Group on Health Systems Performance Assessment, 2017[38]):
Structures to assess the system levers necessary to transition to an integrated care system (e.g. use of digital tools for integration of care among primary care physicians, and share of primary care offices using electronic health records (OECD, 2021[39]))
Processes such as care transitions between and within sectors and task shifting across health professionals
Outcomes by population groups and/or disease areas, self-reported outcomes, as well as utilisation indicators that act as a proxy for health outcomes. See Box 1.6 for further examples.
“Good structure increases the likelihood of good process, and good process increases the likelihood of good outcomes.” (Donabedian, 1988[37])
The SMART framework provides useful information on how to select high-quality integrated care indicators. Criteria within the framework cover relevance, accessibility, reliability, validity, and timeframe, as described in Box 1.6 (OECD, 2022[5]).
Box 1.6. Measuring health outcomes
This box outlines health outcomes that are useful for measuring the impact of integrated care models. It also outlines criteria important to consider when selecting which health outcomes to measure.
Types of health outcomes
Measuring health outcomes enhances the quality of evidence supporting integrated care thereby building support from policy makers, health professionals and patients.
Regarding outcomes, the types of indicators to collect will ultimately depend on the integrated care model under evaluation, with examples listed below:
All-cause and disease‑specific mortality (and mortality after hospitalisation) (see (Barrenho et al., 2022[4]))
All-cause and disease‑specific hospital readmissions (Barrenho et al., 2022[4])
Adverse events
Complications
Disease incidence
Blood pressure
Condition specific clinical measures (e.g. cholesterol control, glycaemic control)
Body mass index
Levels of physical activity (e.g. steps per day, minutes per day or moderate to vigorous exercise)
Falls and other injuries.
In addition to the objective measures of health outlined above, it is important to collect self-reported measures from patients (e.g. patient reported experience measures, PREMs, such as the proportion of patients who have not experienced good care co‑ordination (OECD, 2021[39])), as well as utilisation measures that act as a proxy for outcomes such as avoidable hospitalisations for ambulatory care sensitive conditions.
Selecting high quality indicators
Features of high-quality indicators to measure the impact of integrated care models are below (OECD, 2022[5]):
Importance/relevance/utility: time and resources need to be invested to collect data on any indicator. They should therefore be important and meaningful to evaluate the intervention.
Accessibility/feasibility: data needs to be obtainable, which depends on resource constraints, the availability of the data, and the frequency by which it is made available.
Reliability: indicators should measure the issue or outcome consistently, to allow comparisons over time and between people or groups.
Validity/accuracy/robustness: indicators should accurately measure the concept or event. However, in some cases this is not possible, and proxy measures should be considered (e.g. using income as a proxy for socio‑economic status).
Timeframe: it is important to consider the timeframe in which a change in the indicator can reasonably be expected, and whether this falls within the evaluation study period.
Data measuring changes in outcome indicators should be collected over a period that allows researchers to understand the long-term impact of integrated care models. For example, by setting up continuous monitoring systems that track set indicators over time (i.e. data collection is not part of a once‑off study, but forms part of routine practices) (Tsiachristas and Rutten-van Mölken, 2021[36]). This is important given improvements in chronic disease take time to eventuate.
As discussed under “Digital tools and health information systems”, the collection of robust data over time requires countries to have health information systems that support data linkage and sharing of patient information.
Develop internationally comparable data to measure the impact of integrated care models
Studies measuring the impact of selected integrated care models used a range of indicators. Therefore, it is difficult to assess the relative impact of different integrated care models implemented across OECD and EU27 countries. To understand which integrated models work best and therefore which to scale‑up and transfer, countries should prioritise the collection of internationally comparable data (Report by the Expert Group on Health Systems Performance Assessment, 2017[38]).
As part of its work on integrated care, the OECD have outlined 13 promising internationally-comparable outcome indicators to be routinely collected with a focus on ischaemic stroke and congestive heart failure (CHF) (Barrenho et al., 2022[4]). Indicators relate to either hospital readmissions, mortality, or prescription of appropriate medication for secondary care prevention after hospital discharge. These are calculated for people admitted to the hospital with an acute non-elective (urgent) episode of care for a first-time event of ischaemic stroke or CHF. Data for these indicators submitted by countries used at least seven years of patient-linked datasets from hospitals (inpatient care), emergency care, death registries, and pharmaceutical and prescribing data. (See Chapter 6 of the latest OECD Health at a Glance report for initial findings across 11 OECD countries (OECD, 2021[1])).
The use of several data points from different datasets to measure the impact of integrated care highlights the importance of having governance structures that support data linkage and sharing of patient information (see “Digital tools and health information systems” for further details).
Prioritise economic evaluations of integrated care models
Evidence supporting the economic value of integrated care models is of key importance given tight budgetary constraints in government. Types of economic evaluations, such as cost-utility and cost-effectiveness analyses, are in Box 1.7 with details on factors to consider when developing an economic evaluation study below (Tsiachristas and Rutten-van Mölken, 2021[36]):
The integrated care model under evaluation must be clearly and thoroughly defined. The definition should include information on the setting, target population, intervention components, and duration of the intervention, for example.
Comparator(s) to the integrated care model should be defined – for example, usual care practices and/or alternative models of care.
An appropriate study design should be confirmed at the outset before the model of care is introduced to establish baseline data. Example study designs include observational studies and randomised controlled trials (see OECD’s Guidebook on Best Practices in Public Health for information on the types of study designs available) (OECD, 2022[5]).
Define an evaluation period that is suitable for the benefits of the integrated care model to be realised and ensure baseline data is collected before the model is implemented.
Define appropriate outcome measures, such as those outlined in Box 1.6, which include routinely collected indicators by the OECD as well as new integrated care indicators recently piloted by the OECD (Barrenho et al., 2022[4]).
Define how to measure and value costs such as labour, capital, consumables, administrative and overhead costs, as well as societal costs more broadly. For example, evaluations of telehealth should consider their impact on patient travel and waiting times, both of which result in lost productivity. As an example, research undertaken in Canada found the Canadian Ontario Telemedicine Network reduced patient travel distance by 270 million km in one year, leading to costs savings from a reduction in travel grants by CAD 71.9 million (EUR 50.2 million) (OTN, 2018[40]).
Box 1.7. Types of economic evaluations
An economic evaluation assesses costs in relation to benefits to assist policy makers make decisions that maximise outcomes from a limited set of resources. Commonly applied economic evaluations in the health sector include cost-utility, cost-benefit, cost-effectiveness analysis, and cost-consequence analysis. The appropriate economic evaluation depends on several factors including on how outcomes are measured (OECD, 2022[5]).
Cost-utility analysis (CUA): CUA provides an estimate of the additional monetary cost of obtaining one quality-adjusted life year (QALY) (i.e. one year in full health). CUAs are appropriate when assessing multiple interventions with different objectives, all of which are converted into QALYs.
Cost-benefit analysis (CBA): CBA transforms outcome measures into a monetary unit and compares this with the cost of the intervention (i.e. cost-benefit ratio). It provides a net monetary cost of achieving an additional unit of outcome. It is an appropriate technique when outcomes can be translated into monetary terms.
Cost-effectiveness analysis (CEA): CEA calculates the estimated costs of an additional outcome unit across one or more interventions. The outcome unit is dependent on the intervention being evaluated. CEAs are useful when assessing interventions with the same outcome indicator of interest.
Cost-consequence analysis (CCA): CCA assesses several costs and consequences (i.e. effects) for the intervention under evaluation and reports them separately.
Health equality
Vulnerable populations are at greater risk of experiencing care fragmentation
Vulnerable populations include, but are not limited to, people with a low socio-economic status (SES), older populations, racial and ethnic minorities, and those living in rural and remote areas (OECD, 2022[5]). People in these groups are at greater risk of living with complex health needs for several reasons including lower levels of health literacy thereby making it difficult to navigate the health system, as well as reduced access to healthcare services. For example, across EU27 countries, the proportion of people who report living with a long-standing illness or health problem is 15 percentage points higher among those living in the poorest income quintile compared to those in the richest quintile (43% versus 28%) (Eurostat, 2022[41]).
People with complex health needs often require multiple treatments and interact with several providers. For these reasons, vulnerable populations are at greater risk of “poor quality care, poor health outcomes, and poor experiences of care as a result of fragmentation” (Barrenho et al., 2022[4]).
The needs of vulnerable populations are not always addressed by integrated care models
The importance of designing integrated care models to reduce health inequalities is well recognised. Despite this, only three of the 13 selected case studies have activities in place to address the specific needs of vulnerable populations:
Incorporating new languages into existing services: the Finnish city of Oulu’s patient-provider portal is in the process of adding Arabic, Dari, and Somali languages to its service. Refugees in Finland typically speak these languages. Similarly, the OptiMedis Health Kiosk offers counselling services in Arabic, Farsi, Russian and Polish.
Offering user friendly interfaces: the patient-provider portal in Oulu has also adapted its video platform to include an easy-to‑use function for patients with a disability.
Providing technological support: Scotland’s Technology-Enabled Care (TEC) intervention offers support and funding to ensure older people in care homes have reliable internet connections, devices and other infrastructure needed for digital care.
The remaining case studies may indirectly reduce health inequalities by targeting patients with complex health needs, which, as previously mentioned, are more likely to be vulnerable. However, this assumption is dependent on patients from vulnerable groups having equal access to healthcare in the first place, which is not always supported by real-world evidence among OECD countries. For example, poorer populations are less likely to access preventative care, such as screening, as well as primary care via a visit to their general practitioner (OECD, 2019[42]).
The impact of integrated care models on health inequalities is not adequately assessed
As outlined under “Monitoring and evaluation”, studies measuring the impact of integrated care models focus on patient experience and utilisation of healthcare services. Just one case study, the integrated care model for multimorbidity in the Basque Country, Spain, produced evaluation results disaggregated by different population groups. Specifically, an evaluation by Sorto-Gordoa et al. (2019[43]) found that the most deprived economic group had a higher probability of accessing primary care and a lower probability of utilising hospital services among all participants.
Given the limited amount of data among selected case studies, it is not possible to determine if integrated care models narrow or widen existing health inequalities.
Policy recommendations
Evaluate the impact of integrated care models on different population groups and adapt accordingly
When studying the impact of healthcare interventions, such as integrated care models, it is important to look at their impact on inequalities. Future research should therefore prioritise collecting patient information on variables relevant to assessing inequalities. These variables include (O’Neill et al., 2014[44]):
Gender
Age
Race and ethnicity
Education
Income
Geographical location.
Further details on stratifying data and undertaking rigorous evaluations are available in OECD’s Guidebook on Best Practices in Public Health (OECD, 2022[5]).
Evaluations that stratify findings according to key sociodemographic variables provide important information on how integrated care models affect population groups differently. For example, differences in access to and outcomes from integrated care. This information can subsequently be used to adapt specific integrated care models as well as larger policy plans for integrated care to ensure the needs of vulnerable populations are met.
Promote health literacy among vulnerable populations
Health literacy (HL) refers to an individual’s knowledge, motivation, and skills to access, understand, evaluate, and apply health information. As outlined above, HL is lower among vulnerable populations. For example, a nationwide study of HL in Denmark found immigrants and individuals with basic education and below-average income had lower levels of HL (Svendsen et al., 2020[45]). Activities to promote HL among vulnerable populations have the potential to improve overall population health and narrow existing health inequalities.
Scaling-up and transferability
Only half of all selected case studies have been transferred to another country or scaled-up across the country in which they were originally implemented
Four of the 13 selected case studies have been transferred from their original “owner” country to another “target” country (see Table 1.4). For example, the mHealth app, Mobile Airways Sentinel Network (MASK), operates in 28 countries, most of which are OECD member countries. Further, the United States (California), Luxembourg, the Czech Republic and Norway adopted the nationwide Dutch programme, ParkinsonNet. Most case studies, however, operate within a specific region in a country, either permanently or as a pilot programme. The City of Oulu in Finland, for example, scaled-up the Self Care Service patient portal from a pilot to the whole city in 2011. (See Chapter 5 for further details).
Table 1.4. Scale‑up and transfers of selected integrated care case studies
|
Transferred to another country |
Scaled-up across a whole country |
Scaled-up across a region within a country |
Pilot programme |
|
|---|---|---|---|---|
|
OptiMedis, regionally based integrated care model* |
✓ |
|||
|
Hospital-at-Home |
✓ |
|||
|
Mobile Airways Sentinel Network (MASK) app |
✓ |
|||
|
Oulu Self Care Service (patient portal) |
✓ |
|||
|
Integrated care model for multimorbidity, Basque Country |
✓ |
✓ |
||
|
Badalona Healthcare Services |
✓ |
|||
|
Medical Diagnostic Centre |
✓ |
|||
|
TeleHomeCare in the Italian city of Ceglie Messapica |
✓ |
|||
|
Digital Roadmaps towards an integrated healthcare system |
✓ |
✓ |
||
|
Technology Enabled Care (TEC) |
✓ |
|||
|
Telemonitoring for patients with advanced heart failure |
✓ |
|||
|
ParkinsonNet |
✓ |
✓ |
||
|
Personalised Actions Plans |
✓ |
Note: *There are active discussions in regions of France (Strasbourg) and Belgium (Germany speaking community) to transfer this model of care as part of the EU Joint Action on implementation of digitally enabled person-centred care (JADECARE).
Although most selected case studies were not widely scaled-up or transferred, they are, in most cases, based on a well-known model of care. For example:
The City of Oulu’s patient portal: patient portals are increasingly common in OECD and EU27 countries; based on a 2016 EHR survey, 12 (out of 15) OECD countries reported they have or are in the process of implementing a patient portal (OECD, 2019[28]).
The Basque Country’s integrated care model of multimorbidity and Poland’s Medical Diagnostic Centres (MDC): 17 OECD member countries have developed “new models of primary care” that promote care integration. Like the Basque Country’s integrated care model and Poland’s MDC, these new models of care offer (OECD, 2020[3]):
Multidisciplinary practices or inter-professional practices
Comprehensive health services in the community
Population health management (generally based on risk stratification using sophisticated IT systems, although not in the case of MDC)
Engage patients in shared decision-making.
Personalised Actions Plans in Andalusia, Spain: personalised care plans have been widely used across developed countries for many years including in Australia, England (United Kingdom) and even different regions of Spain (OECD, 2020[3]).
Hospital-at-Home, Catalonia, Spain: healthcare systems increasingly provide post-discharge care at home as an alternative to hospital-based care. Example countries include Australia, Canada, Germany, Israel, and the United Kingdom.
Telemonitoring for Advanced Heart Failure (HF), Olomouc, the Czech Republic: Sweden, Spain and Japan have national-level telemonitoring programmes for HF patients, while pilot interventions operate in countries such as Austria, Denmark, Portugal and the United Kingdom.
TeleHomeCare, Ceglie Messapica, Italy: similar telemonitoring programmes are in place in many countries either at the local, regional or national level, for instance, the Ontario Telemedicine Network in Canada (Oliveira Hashiguchi, 2020[32]).
International programmes assist the cross-country transfer of best practice integrated care models
Several of the selected case studies have or currently participate in international programmes dedicated to transferring best practice integrated care models. These programmes include the Joint Action on implementation of digitally enabled integrated person-centred care (JADECARE), SCIROCCO (Scaling Integrated Care in Context) Exchange project, Digital Health Europe Twinning Project, and the European Innovation Partnership on Active and Health Ageing (EIP-AHA) Twinning Project. Box 1.8 outlines how selected case studies were involved in these programmes.
Box 1.8. International programmes to transfer best practice integrated care models
Listed below are EU-funded projects to promote the transfer of best practice integrated care models.
JADECARE
JADECARE is an EU initiative designed to help Member States make the transition to digitally-enabled and integrated, person-centred care. Under the Joint Action, “early adopters” of original good practice interventions support “next adopters” to transfer the integrated care model to their local setting.
Four of the 13 selected case studies are early adopters of good practice interventions, as summarised below:
Specific features of the OptiMedis Model will be transferred to six regions in Europe.
Hospital-at-Home within the Catalan Open innovation on ITC-supported integrated care services for chronic patients will be transferred to five regions in Europe.
Specific features of the integrated care model for multimorbid patients, the Basque Country, Spain will be transferred to nine European regions. Specifically, regions in Bosnia and Herzegovina, Croatia, the Czech Republic, Denmark, Greece, Italy (two regions) Portugal and Serbia.
Specific interventions within Southern Denmark’s Digital Roadmaps programme will be transferred to nine Member States in Europe. Next adopters participated in a study visit where the owners of the intervention in Denmark presented the transferability of individual interventions that make up the initiative.
SCIROCCO Exchange Project
Technology-Enabled Care (TEC) in Scotland participated in the SCIROCCO Exchange project – a project that aims to support health and social care authorities to adopt and scale‑up integrated care models.
EIP-AHA Twinning Project
As part of the EIP-AHA Twinning Project, the MASK-air app is being transferred to 25 reference sites. A reference site may be a country, region, or organisation. The purpose of the Twinning Project is to assess the transferability of MASK-air to a range of different contexts and to better understand the burden, diagnosis, and management of rhinitis.
Digital Health Europe funded Twinning Project
As part of a Digital Health Europe‑funded Twinning project, the Scottish TEC programme shared good practices from Scotland with the University of Agder (Norway), Grimstad Kommune (Norway) and the Agency for Social Services and Dependency of Andalusia (Spain), and vice versa.
Policy recommendations
Utilise existing frameworks to assist the transfer of best practice integrated care models
The design, implementation and delivery of integrated care models involve multiple stakeholders across different levels of health and social care systems. Transferring such models of care within and across countries is therefore complex.
Several publicly available frameworks to begin the process of scaling-up or transferring an integrated care model are available. These frameworks assist stakeholders to compile information to assess whether the model of care can be transferred and, if so, what steps need to be taken to adapt the model to the local setting. Box 1.9 describes a selection of frameworks identified as part of this review.
Box 1.9. Frameworks for scaling-up and transferring integrated care models
Described below are three publicly available frameworks to assist the transfer of integrated care models.
OECD’s Transferability Framework within the Guidebook of Best Practices in Public Health
OECD’s Guidebook on Best Practices in Public Health outlines four contextual factors that affect the successful transfer of an intervention (OECD, 2022[5]):
Population context: covers population characteristics, sociodemographic factors as well as broader cultural considerations. For example, does the model of care align with population health needs?
Sector specific context: governance/regulation, financing, workforce, capital (including technological infrastructure) and access arrangements.
Political context: political will from policy makers to implement integrated care models.
Economic context: whether implementing and operating the integrated care model is affordable in the long run.
The SCIROCCO Maturity Model for Integrated Care
Scaling Integrated Care in Context (SCIROCCO) is a project co-funded by the European Commission which aims to adopt and transfer good practices in integrated care. A key output of SCIRICCO is the Maturity Model which outlines 12 dimensions necessary for assessing areas of strength and weakness in regard to implementing integrated care (SCIROCCO, n.d.[46]). Outcomes from the self-assessment determine the readiness of care authorities to adopt integrated care and supports authorities improve their capacity to deploy integrated care (Report by the Expert Group on Health Systems Performance Assessment, 2017[38]).
The 12 dimensions are capacity building, readiness to change, structure and governance, information and eHealth services, financing and funding, standardisation and simplification, removal of inhibitors, population approach, citizen empowerment, evaluation methods, breadth of ambition, innovation management and capacity building (SCIROCCO, n.d.[46]).
The MAST Model (Model of Assessment of Telemedicine)
The MAST Model is a tool designed to evaluate telemedicine interventions. The model consists of three steps the first of which assesses the “maturity of the telemedicine technology and the organisation using the service” (Kidholm et al., 2012[47]). Specifically, step one obtains a view of patient characteristics, primary outcomes and whether the telemedicine approach can be compared with usual care, an upgraded system or different technology, and identified barriers and issues including legislation (national and regional level), reimbursement (how services are paid for), maturity, and number of patients.
Develop close ties between the owner and adopter of best practice integrated care models
A review of health promotion intervention transfers as part of the EU’s Joint Action on Chronic Diseases found building a “strong relationship between the good practice owner and implementer” was a key transfer facilitator (Stegeman et al., 2020[48]). This finding aligns with feedback from owners of selected cases studies who highlighted the importance of sharing “lessons learnt” and “core features” of their best practice model. Examples of how to facilitate the transfer of selected case studies are below, several of which highlight the importance of local authorities in spreading best practice models of care:
The transfer of ParkinsonNet from the Netherlands to the German region of Niederrhein identified several valuable lessons from the failure of the intervention to “take off”. Specifically, the need for a “champion” with expertise in Parkinson’s disease to promote the programme, a “super trouper” who receives ongoing training and educates other trainers, and lastly a “business case” to capitalise on healthcare savings made by the programme.
Administrators of the Personalised Action Plans (PAPs) in Andalusia, Spain, shared key factors to consider before transferring PAPs. These factors include having a team of experts to develop training materials on how to treat patients with complex needs, ensuring there is sufficient training for health professionals and patients, linking PAPs with patient EHRs, and ensuring health professionals have the time and resources to develop PAPs.
Administrators of the Hospital-at-Home programme in Catalonia, Spain, identified three key factors necessary for the successful transfer of the programme: strong and supportive leadership at the hospital level, a culture of integrated care, and reimbursement arrangements that incentivise care delivered in a home setting.
Administrators of the integrated care organisation in the Spanish municipality of Badalona outlined several transfer facilitators regarding integrated care models that bring together health and social care. These facilitators cover policy, governance, workforce and culture, and digital tools (see Box 1.10).
International transfer projects, such as those outlined in Box 1.9, help build ties between implementers and adopters, and therefore create an international learning network. (See Chapters 3 to 15 for further details on each case study mentioned above).
Box 1.10. Case study: transfer facilitators of integrated healthcare organisations, Badalona, Spain
This box outlines facilitators for transferring integrated care models that bring together health and social care. The facilitators are broken into four categories: policy, governance, workforce and culture, and digital tools. Facilitators were identified by administrators of Badalona’s integrated care organisation.
Policy
Strong policy commitment towards providing patient-centric care
Ensure the views of all key stakeholders are included – e.g. research organisations, policy makers, service providers and end-users
Governance
One governance and organisational structure for health and social care services – without such a structure, implementation costs are likely to be very high given the change required for institutional, organisation, cultural and legal arrangements
Implementation is more straightforward in countries with national health systems as opposed to insurance‑based models
Involvement of as many stakeholders as possible in terms of horizontal governance
Workforce and culture
Allowing health and social care providers to play a leading role in developing and implementing this new model of care
Willingness and motivation among the workforce to implement such models of care
Culture of innovation
Involvement of young people given they tend to be more innovative, experience fewer cultural constraints and have good ideas
Digital tools
Sophisticated health information system, including wide‑spread use of EHRs that allow for efficient communication across the spectrum of care
No resistance to health technology among patients and providers
Source: Vallis, Piera and Tolra (n.d.[49]), “Report of in depth analysis of Badalona Healthcare services (BSA)” case study”; Vallive et al. (2016[50]), “SELFIE 2020: Work Package 2: Thick descriptions of the two Catalan case studies, Badalona Serveis Assistencials (BSA) (Spain)”; Lupiañez-Villanueva and Theben (2015[51]), “Strategic Intelligence Monitor on Personal Health Systems Phase 3 (SIMPHS3): BSA (Spain) Case Study Report”.
References
[27] American Public Health Association (2022), Community Health Workers, https://www.apha.org/apha-communities/member-sections/community-health-workers.
[7] Barrenho, E., R. Fujisawa and C. Kendir (2020), Strengthening Performance of Integrated Care Delivery across OECD countries, Issues Note 28th Session of the OECD Health Committee.
[4] Barrenho, E. et al. (2022), “International comparisons of the quality and outcomes of integrated care: Findings of the OECD pilot on stroke and chronic heart failure”, OECD Health Working Papers, No. 142, OECD Publishing, Paris, https://doi.org/10.1787/480cf8a0-en.
[34] Baxter, S. et al. (2018), “The effects of integrated care: a systematic review of UK and international evidence”, BMC Health Services Research, Vol. 18/1, https://doi.org/10.1186/s12913-018-3161-3.
[25] Berini, C., H. Bonilha and A. Simpson (2021), “Impact of Community Health Workers on Access to Care for Rural Populations in the United States: A Systematic Review”, Journal of Community Health, Vol. 47/3, pp. 539-553, https://doi.org/10.1007/s10900-021-01052-6.
[37] Donabedian, A. (1988), “The quality of care. How can it be assessed?”, JAMA: The Journal of the American Medical Association, Vol. 260/12, pp. 1743-1748, https://doi.org/10.1001/jama.260.12.1743.
[41] Eurostat (2022), Database - Eurostat, https://ec.europa.eu/eurostat/data/database (accessed on 15 March 2022).
[29] Fahy, N. and G. Williams (2021), Use of digital health tools in Europe: Before, during and after COVID-19, European Observatory on Health Systems and Policies, Policy brief 42.
[21] Hanson, K. et al. (2022), “The Lancet Global Health Commission on financing primary health care: putting people at the centre”, The Lancet Global Health, Vol. 10/5, pp. e715-e772, https://doi.org/10.1016/s2214-109x(22)00005-5.
[17] Hughes, L., M. McMurdo and B. Guthrie (2012), “Guidelines for people not for diseases: the challenges of applying UK clinical guidelines to people with multimorbidity”, Age and Ageing, Vol. 42/1, pp. 62-69, https://doi.org/10.1093/ageing/afs100.
[12] Izagirre-Olaizola, J., G. Hernando-Saratxaga and M. Aguirre-García (2021), “Integration of health care in the Basque Country during COVID-19: the importance of an integrated care management approach in times of emergency”, Primary Health Care Research & Development, Vol. 22, https://doi.org/10.1017/s146342362100044x.
[47] Kidholm, K. et al. (2012), “A model for assessment of telemedicine applications: MAST”, International Journal of Technology Assessment in Health Care, Vol. 28/1, pp. 44-51, https://doi.org/10.1017/s0266462311000638.
[26] Kim, K. et al. (2016), “Effects of Community-Based Health Worker Interventions to Improve Chronic Disease Management and Care Among Vulnerable Populations: A Systematic Review”, American Journal of Public Health, Vol. 106/4, pp. e3-e28, https://doi.org/10.2105/ajph.2015.302987.
[24] Kim, K. et al. (2016), “Community Health Workers Versus Nurses as Counselors or Case Managers in a Self-Help Diabetes Management Program”, American Journal of Public Health, Vol. 106/6, pp. 1052-1058, https://doi.org/10.2105/ajph.2016.303054.
[19] Leach, B. et al. (2017), “Primary care multidisciplinary teams in practice: a qualitative study”, BMC Family Practice, Vol. 18/1, https://doi.org/10.1186/s12875-017-0701-6.
[16] Lindner, L. and L. Lorenzoni (forthcoming), “Innovative providers’ payment models for promoting value-based health systems: Start small, prove value, and scale up”, OECD Health Working Papers, OECD Publishing, Paris.
[23] Looman, W. et al. (2021), “Drivers of successful implementation of integrated care for multi-morbidity: Mechanisms identified in 17 case studies from 8 European countries”, Social Science & Medicine, Vol. 277, p. 113728, https://doi.org/10.1016/j.socscimed.2021.113728.
[8] Lorenzoni, L. and R. Milstein (2022), “Value-based providers’ payment models: understanding where and under which conditions they work”, OECD, Paris, https://www.oecd.org/health/Value-based-providers-payment-models.pdf.
[51] Lupiañez-Villanueva, F. and A. Theben (2015), Strategic Intelligence Monitor on Personal Health Systems Phase 3 (SIMPHS3): BSA (Spain) Case Study Report.
[13] Mateo-Abad, M. et al. (2020), “Impact of the CareWell integrated care model for older patients with multimorbidity: a quasi-experimental controlled study in the Basque Country”, BMC Health Services Research, Vol. 20/1, https://doi.org/10.1186/s12913-020-05473-2.
[10] Ministry of Health and Consumer Affairs (2010), A Strategy to Tackle the Challenge of Chronicity in the Basque Country, https://ec.europa.eu/eip/ageing/sites/eipaha/files/practices/chronicitybasquecountry.pdf.
[33] National Digital Inclusion Alliance (2022), Definitions, https://www.digitalinclusion.org/definitions/#.
[5] OECD (2022), Guidebook on Best Practices in Public Health, OECD Publishing, Paris, https://doi.org/10.1787/4f4913dd-en.
[30] OECD (2022), Healthy Eating and Active Lifestyles: Best Practices in Public Health, OECD Publishing, Paris, https://doi.org/10.1787/40f65568-en.
[1] OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en.
[39] OECD (2021), Health for the People, by the People: Building People-centred Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/c259e79a-en.
[3] OECD (2020), Realising the Potential of Primary Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/a92adee4-en.
[42] OECD (2019), Health for Everyone?: Social Inequalities in Health and Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/3c8385d0-en.
[28] OECD (2019), Health in the 21st Century: Putting Data to Work for Stronger Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/e3b23f8e-en.
[31] OECD (2019), Individuals using the Internet for seeking health information - last 3 m (%) (all individuals aged 16-74), Dataset: ICT Access and Usage by Households and Individuals.
[14] OECD (2018), Policy Survey on the Future of Primary Care, and OECD: Health System Characteristics Survey, OECD, Paris.
[20] OECD (2016), Health Systems Characteristics Survey 2016, https://qdd.oecd.org/subject.aspx?Subject=hsc.
[2] OECD (forthcoming), Maintaining Care Continuity, OECD, Paris.
[32] Oliveira Hashiguchi, T. (2020), “Bringing health care to the patient: An overview of the use of telemedicine in OECD countries”, OECD Health Working Papers, No. 116, OECD Publishing, Paris, https://doi.org/10.1787/8e56ede7-en.
[44] O’Neill, J. et al. (2014), “Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health”, Journal of Clinical Epidemiology, Vol. 67/1, pp. 56-64, https://doi.org/10.1016/j.jclinepi.2013.08.005.
[40] OTN (2018), OTN Annual Report 2017/18, https://otn.ca/wp-content/uploads/2017/11/otn-annual-report.pdf.
[22] Ranjan, P. (2015), “How can Doctors Improve their Communication Skills?”, Journal of Clinical and Diagnostic Research, https://doi.org/10.7860/jcdr/2015/12072.5712.
[38] Report by the Expert Group on Health Systems Performance Assessment (2017), Blocks: Tools and methodologies to assess integrated care in Europe, European Commission, https://health.ec.europa.eu/publications/blocks-tools-and-methodologies-assess-integrated-care-europe_en.
[35] Rocks, S. et al. (2020), “Cost and effects of integrated care: a systematic literature review and meta-analysis”, The European Journal of Health Economics, Vol. 21/8, pp. 1211-1221, https://doi.org/10.1007/s10198-020-01217-5.
[18] Saint-Pierre, C., V. Herskovic and M. Sepúlveda (2017), “Multidisciplinary collaboration in primary care: a systematic review”, Family Practice, Vol. 35/2, pp. 132-141, https://doi.org/10.1093/fampra/cmx085.
[46] SCIROCCO (n.d.), Maturity Model, https://www.scirocco-project.eu/maturitymodel/ (accessed on 9 December 2020).
[43] Soto-Gordoa, M. et al. (2019), “Gender and socioeconomic inequalities in the implementation of the Basque programme for multimorbid patients”, European Journal of Public Health, Vol. 29/4, pp. 681-686, https://doi.org/10.1093/eurpub/ckz071.
[48] Stegeman, I. et al. (2020), D5.3 Recommendations for the implementation of health promotion good practices: Building on what works: transferring and implementing good practice to strengthen health promotion and disease prevention in Europe, EuroHealthNet & Finnish Institute for Health and Welfare.
[15] Struckmann, V. et al. (2016), How to strengthen financing mechanisms to promote care for people with multimorbidity in Europe? Policy Bried 24, European Observatory on Health Systems and Policies.
[45] Svendsen, M. et al. (2020), “Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large national population-based survey among Danish adults”, BMC Public Health, Vol. 20/1, https://doi.org/10.1186/s12889-020-08498-8.
[11] The CareWell Group (2018), “Impact of stratification on the effectiveness of a comprehensive patient-centered strategy for multimorbid patients”, Health Services Research, Vol. 54/2, pp. 466-473, https://doi.org/10.1111/1475-6773.13094.
[36] Tsiachristas, A. and M. Rutten-van Mölken (2021), “Economic Evaluation of Integrated Care”, in Handbook Integrated Care, Springer International Publishing, Cham, https://doi.org/10.1007/978-3-030-69262-9_34.
[49] Valls, A., J. Piera and J. Tolra (n.d.), Report of in depth analysis of Badalona Healthcare services (BSA)” case study.
[50] Vallve, C. et al. (2016), SELFIE 2020: Work Package 2: Thick descriptions of the two Catalan case studies, Badalona Serveis Assistencials (BSA) (Spain).
[9] Vallve, C. et al. (2016), Work Package 2 Report: Spain, SELFIE 2020, https://www.selfie2020.eu/wp-content/uploads/2016/12/SELFIE_WP2_Spain_Final-thick-descriptions.pdf.
[6] Wodchis, W. et al. (2020), “Innovative Policy Supports For Integrated Health And Social Care Programs In High-Income Countries”, Health Affairs, Vol. 39/4, pp. 697-703, https://doi.org/10.1377/hlthaff.2019.01587.
Notes
← 1. Norway has introduced several add-on payments to incentivise integrated care. For example, an add-on tariff to the existing DRG-based activity financing system that is dedicated to specialised treatment provided outside the hospital/patient clinic (e.g. at a patient’s home or long-term care facility). Specialised treatment here refers to mental health and drug abuse treatment (introduced in 2017) and somatic care (introduced in 2018). Other examples of add-on payments in Norway include a DRG for collaborative activities between hospital and other institutions (e.g. social services and schools) and a results-based financing scheme targeting specialised healthcare services.
← 2. These payment models are also referred to as “population-based payment models”.
← 3. The level of government most appropriate to facilitate data linkages is context specific and will therefore differ across countries.