Being overweight or obese is a major risk factor for various non-communicable diseases, including diabetes, cardiovascular diseases, and certain cancers. During the pandemic, obesity increased the risk of severe symptoms, as well as the risk of COVID‑19 related hospitalisation and death (OECD, 2023[1]). Women and men with lower incomes are more likely to be obese, entrenching health inequalities. High consumption of energy‑dense food, trans-fats and saturated fats, and increasingly sedentary lifestyles have contributed to growing global obesity rates. Unfavourable shifts in eating behaviours and physical activity patterns were accentuated by the mobility restrictions during the pandemic, potentially counteracting the gains made by policies promoting healthier lifestyles and accentuating the prevalence of obesity (WHO Regional Office for Europe, 2022[2]).
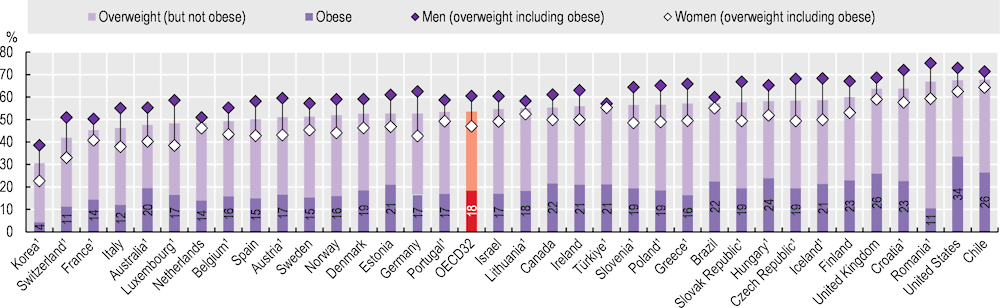
In most OECD countries that collect self-reported body height and weight data, more than half of adults were overweight or obese. On average across 32 OECD countries, 54% of the adult population were overweight or obese, and 18% were obese in 2021. Men were more likely than women to be overweight or obese in all countries. The gender gap was particularly large in Luxembourg, Germany and the Czech Republic (a difference of 19‑20 percentage points) (Figure 4.12).
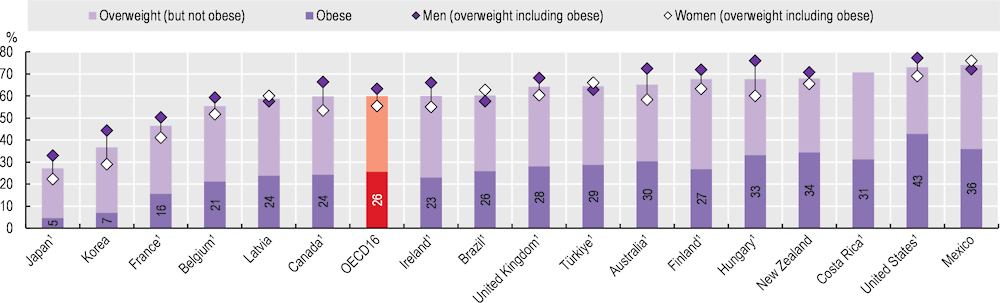
Measured height and weight data are a more reliable indicator but are available for a narrower set of countries. Across the 16 OECD countries with measured data, 60% of adults were overweight or obese, and 26% were obese in 2021 or in the latest available year (Figure 4.13). In 13 of these 16 countries, over half of the adult population was overweight or obese. For Mexico, the United States and Costa Rica, this proportion exceeded 70%. Conversely, in Japan and Korea, fewer than 40% of adults were overweight or obese. Men were more likely than women to be overweight or obese in most countries, except in Latvia, Mexico and Türkiye. The gender gap was relatively wide in Australia, Hungary and Korea (a difference of 14‑16 percentage points).
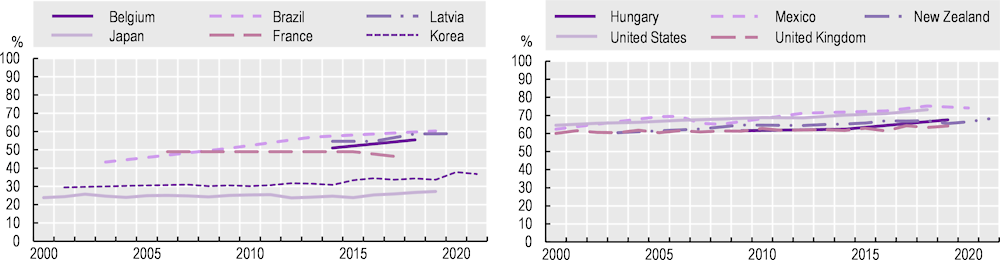
The proportion of overweight and obese adults has increased since the early 2000s in most OECD countries. In most countries where rates were historically low, such as Japan, Korea, Latvia and Belgium, as well as partner country Brazil, overweight and obesity rates grew by 1‑2% annually (Figure 4.14, left panel), although in France, overweight and obesity rates decreased slightly between 2006 and 2017. In countries with relatively high proportions of overweight and obese adults, the rates have also increased – by around 1% annually in Hungary, Mexico, New Zealand and the United States (Figure 4.14, right panel). Overweight and obesity rates increased at a relatively slow pace in the United Kingdom.
Overweight and obesity rates among adolescents are also major public health concerns: 18.3% of adolescents aged 15 years were overweight or obese in 2017‑18 on average across 27 OECD countries. Social inequalities were visible in all these countries, and boys were always more likely to be overweight than girls. The proportion of 15‑year‑olds who were overweight or obese has increased in 23 of these 27 countries since 2009‑10 based on data from the Health Behaviour in School-aged Children survey (Inchley et al., 2020[3]).
OECD member countries have implemented a suite of regulatory and non-regulatory initiatives to reduce overweight population rates. Prominent examples include mass media campaigns to promote the benefits of healthy eating; promotion of nutritional education and skills; taxes on energy-dense food and drink items to discourage consumption; simplified food labelling to communicate nutritional value; and agreements with the food industry to improve the nutritional value of products. A number of countries’ “best practice” initiatives, including food labelling, lifestyle counselling, school- and community-based programmes to promote healthy eating and active lifestyles, were evaluated as effective and efficient in reducing overweight and obesity, and were assessed for transferability to other national contexts (OECD, 2022[4]).