Safe prescribing of medicines can be used as an indicator of healthcare quality, complementing information on consumption and expenditure on pharmaceuticals (see Chapter 9). The overuse, underuse or misuse of prescription medicines can lead to serious consequences for the health of the patient and wasteful expenditure. This is the case for opioids and antibiotics, for example.
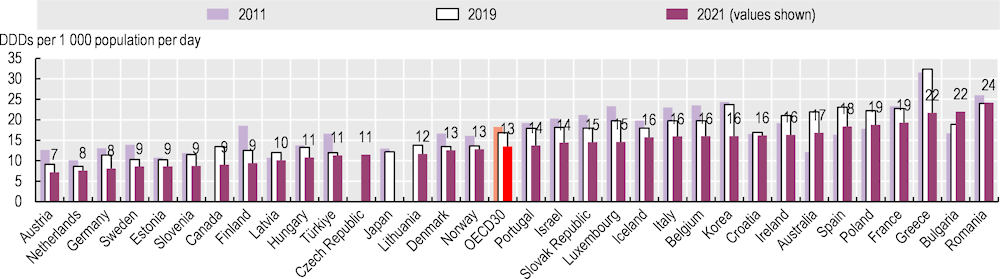
Guidelines recommend that antibiotics should only be prescribed where there is a need that is clearly supported by evidence, to reduce the risk of developing resistant strains of bacteria. The total volume of antibiotics prescribed has been validated as an indicator of quality in the primary care setting, given the rising public health concern caused by antimicrobial resistance across OECD countries (OECD, 2018[1]).
Figure 6.6 shows the overall volume of antibiotics prescribed in 2021, compared to 2019 and 2011. On average, 13 defined daily doses (DDDs) of antibiotics per 1 000 population were prescribed across OECD countries in 2021 – a reduction in the overall volume prescribed from 18 DDDs in 2011 and 17 DDDs in 2019. The total volume of antibiotics prescribed in 2021 varied three‑fold across OECD countries, with Austria, the Netherlands and Germany reporting the lowest volumes per population, and Greece, France, Poland and Spain reporting the highest, and with OECD accession countries Romania and Bulgaria higher still. The observed variation might be explained, on the supply side, by differences in the guidelines and incentives that govern primary care prescribers and, on the demand side, by differences in attitudes and expectations regarding optimal treatment of infectious illness. In addition to stricter guidelines and changes in medical practice, in the most recent period, this is probably due to a decrease in cases of infectious diseases thanks to the increased safety measures associated to the COVID‑19 pandemic, such as handwashing, use of face masks and a reduction in overall social interaction.
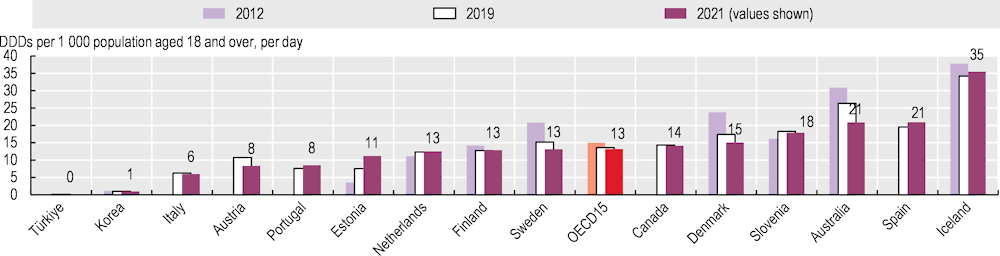
Opioids are used to treat acute pain, such as pain associated with cancer. However, over the last decade opioids have increasingly been used to treat chronic pain, despite the risk of dependence and addiction, leading to serious health risks and often culminating in death. Opioid use is now causing an alarming and rising epidemic of overdose deaths in some OECD countries, such as the United States and Canada (OECD, 2019[2]).
Figure 6.7 indicates that, across OECD countries, the average volume of opioids prescribed in primary care settings in 2021 was 13 DDDs per 1 000 adult population. Iceland reported volumes almost three times the OECD average, at 35 DDDs per 1 000 adult population; Türkiye and Korea reported the lowest volumes, at 1 DDD or less. The wide variation can be explained in part by differences in clinical practice in pain management, as well as differences in regulation, legal frameworks for opioids, prescribing policies and treatment guidelines. Most countries providing data reported a slight decrease in the overall volume of opioids prescribed in 2021 compared to 2019, continuing the downward trend observed from 2012. However, deaths from opioid use remain a major public health concern – particularly in the United States (see section on “Illicit drug use” in Chapter 4).
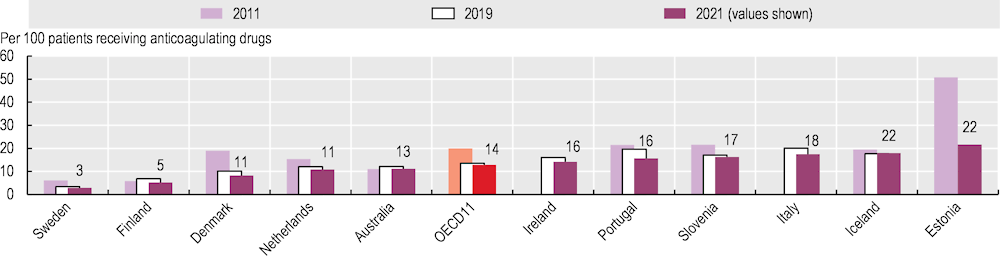
Anticoagulating drugs aim to prevent the formation of blood clots. However, when they are prescribed in combination with oral non-steroidal anti‑inflammatory drugs (NSAIDs), the probability of an adverse bleeding event occurring is higher, thereby limiting the effect of anticoagulant drugs on preventing strokes. Physicians and policy makers should consequently be aware that people receiving anticoagulating drugs should be protected from the risks of combining them with NSAID prescriptions (Penner et al., 2022[3]).
Figure 6.8 shows the proportion of patients with long-term prescriptions of any anticoagulating drug in combination with an oral NSAID among all those receiving anticoagulating drugs. This proportion varies across countries, from Sweden and Finland at 2.9% and 5.2% to Estonia, Iceland, Italy, Slovenia and Portugal, with a proportion above 15%. Across OECD countries as a whole, this proportion has been decreasing since 2011, when it was at 17%, to 15% in 2019, and more recently to 13% in 2021.