Vaccines are a cost-effective tool for protecting against infectious diseases. There is broad agreement within the global scientific community that the most effective way to defeat infectious diseases such as diphtheria, tetanus and pertussis (DTP), measles, hepatitis B, and influenza is through the mass vaccination of populations around the world. High national coverage rates, however, may not be sufficient to stop disease spreading if vaccination rates are uneven within the country, or if take‑up is low in specific population groups. Hence, government action to garner trust and public confidence in the safety and efficacy of vaccination across all population groups is essential for the success of vaccination programmes (OECD, 2021[1]).
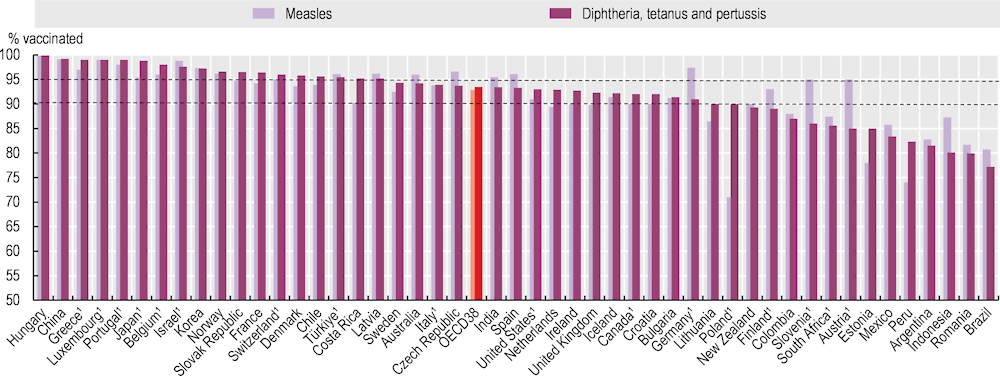
Figure 6.1 shows vaccination coverage for DTP and measles at 1 year of age. Across OECD countries, vaccination rates are high, with around 93% of children on average receiving the recommended DTP and measles vaccinations in 2022. Despite high overall rates for measles, nearly half of countries fall short of the minimum immunisation levels (95%) recommended by the World Health Organization (WHO) to prevent the spread of the disease. Rates of immunisation for measles, which is often incorporated with rubella and/or mumps vaccination are particularly low in Poland (71%) and Estonia (78%). With regards to DTP, almost one in five OECD countries do not meet the minimum immunisation level recommended by WHO (90%), and the immunisation rate is particularly low in Mexico (83%).
Generally, children’s vaccination rates for DTP and measles declined slightly (by less than 2 percentage points) between 2019 and 2022 across OECD countries. This may reflect wavering public confidence in vaccination during the pandemic. Compared to 2015, rates of population perception of the importance of vaccines for children had declined by more than a third in Korea (reaching 48%) and Japan (54%) by 2022 (UNICEF Innocenti, 2023[2]). In the European Union (EU), the percentage of people with confidence in vaccination against measles, mumps and rubella was 85% in 2022, down from 88% in 2020. In Europe, younger people are becoming less confident about vaccinations, and this could lead to further declines in the uptake of children’s routine immunisation (Figueiredo et al., 2022[3]).
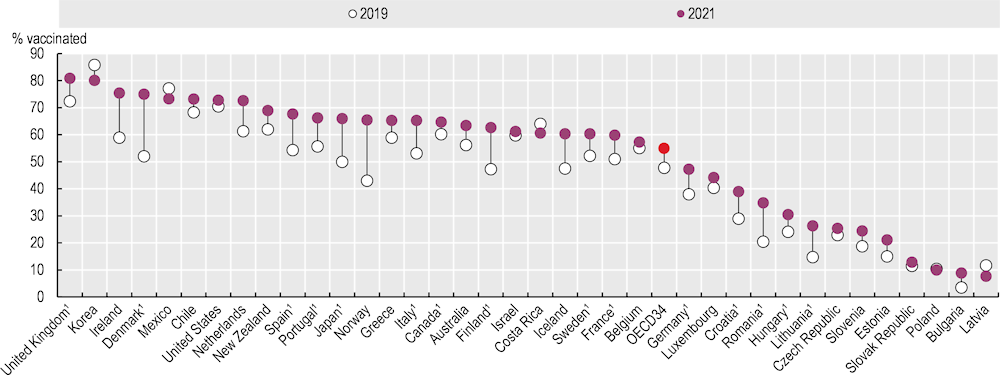
Influenza is a common infectious disease, responsible for 3‑5 million severe cases worldwide each year, along with up to 650 000 deaths (WHO, 2019[4]). As with many countries, the United States saw the number of influenza cases drop significantly from the start of the COVID‑19 pandemic, with the 2021‑22 season recording the lowest level for the last decade. In the EU, however, the 2021‑22 season signalled a return to increased influenza virus activity after the low-level circulation during the pandemic. Since older people are at greater risk of developing serious complications from influenza – such as pneumonia and sepsis, which can result in serious illness or death – WHO recommends that 75% of people aged 65 and over should be vaccinated against seasonal influenza.
Figure 6.2 shows that the WHO target of 75% was only attained in the United Kingdom (81%), Korea (80%) and Denmark and Ireland (75%) in 2021, whereas the influenza immunisation rate among this vulnerable group was very low at below 15% in Latvia, Poland and the Slovak Republic, and also in OECD accession country Bulgaria.
Unlike childhood immunisation, influenza vaccination rates for people aged 65 and over increased to 55% on average across OECD countries in 2021, from 48% in 2019, reflecting increasing public confidence in the flu vaccination in recent years – for example, in most European countries (Figueiredo et al., 2022[3]). The increase in vaccination rates is most notable in Denmark and Norway, with around a 20 percentage point increase since 2019. There were some exceptions to this overall trend, however, with vaccination rates decreasing in Costa Rica, Latvia, Korea and Mexico, by around 5 percentage points in recent years.