Stroke is a leading cause of death, accounting for 6% of all deaths across OECD countries in 2021 (see sections on “Main causes of mortality” and “Mortality from circulatory diseases” in Chapter 3). A stroke occurs when the blood supply to a part of the brain is interrupted, leading to necrosis (cell death) of the affected part. Of the two types of stroke, about 85% are ischaemic (caused by clotting) and 15% are haemorrhagic (caused by bleeding).
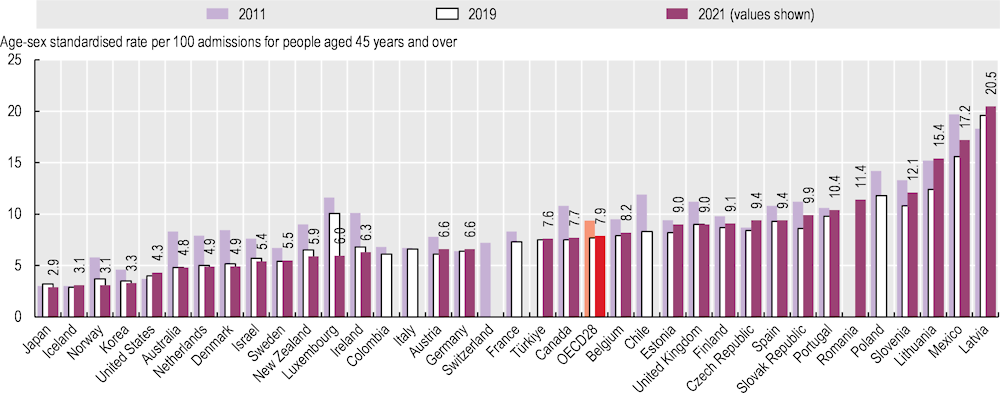
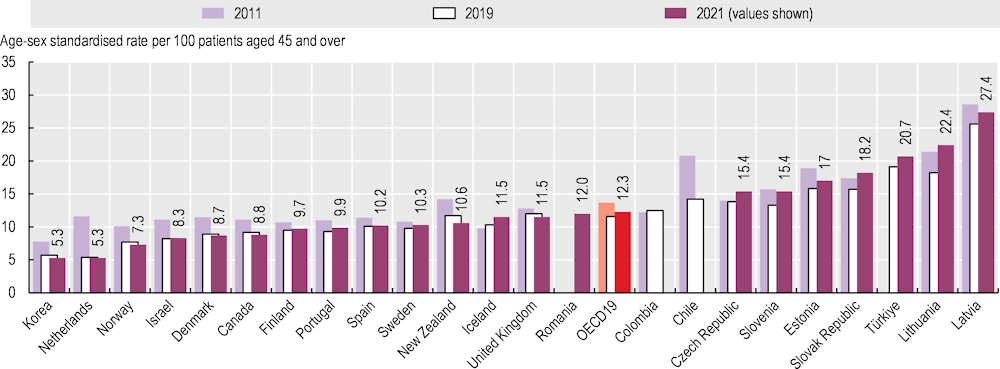
Figure 6.25 shows the case fatality rates within 30 days of hospital admission for ischaemic stroke where death occurred in the same hospital as the initial admission (unlinked data). Figure 6.26 shows the case fatality rate where deaths are recorded regardless of where they occurred, including in another hospital or outside the hospital where the stroke was first recorded (linked data). The indicator using linked data is more robust because it captures fatalities more comprehensively than the same‑hospital indicator, but it requires a unique patient identifier and the capacity to link data, which are not available in all countries. The results from this indicator are higher than for the same‑hospital indicator, as deaths are recorded regardless of where they occurred after hospital admission.
Across OECD countries, almost 8.0% of patients died within 30 days of hospital admission for ischaemic stroke in 2021 using unlinked data (Figure 6.25). The case fatality rates were highest in Latvia, Mexico, Lithuania and Slovenia – all with mortality rates over 11%. Rates were lower than 4% in Japan, Iceland, Norway and Korea. Low rates in Japan are due in part to efforts dedicated to improving the treatment of stroke patients in hospitals, through systematic blood pressure monitoring, major material investment in hospitals and establishment of specialised stroke units (OECD, 2015[1]).
Across 19 OECD countries that reported linked data, 12.3% of patients on average died within 30 days of being admitted to hospital for stroke in 2021 (Figure 6.26). The mortality rate was highest (over 20%) in Türkiye, Lithuania and Latvia, and lowest (under 8%) in Korea, the Netherlands and Norway. Korea has attained a low mortality rates through improvements in acute ischaemic stroke management, including an increased number of comprehensive stroke centres supporting high-quality care and thrombectomy, and expansions in health insurance coverage in relation to mechanical thrombectomy (Park et al., 2022[2]).
Treatment for ischaemic stroke has advanced dramatically over recent decades, with systems and processes now in place in many OECD countries to identify suspected ischaemic stroke patients and to deliver acute reperfusion therapy quickly. Between 2011 and 2019, case fatality rates for ischaemic stroke decreased across OECD countries: from 9.4% to 7.7% for unlinked data rates and from 13.7% to 11.6% for linked data rates (Figure 6.25 and Figure 6.26). Countries can improve the quality of stroke care further through timely transportation of patients, evidence‑based medical interventions and access to high-quality specialised facilities such as stroke units (OECD, 2015[1]). Advances in technology are leading to new models of care to deliver reperfusion therapy even more quickly and efficiently, whether through pre‑hospital triage by telephone or administering the therapy in the ambulance.
Between 2019 and 2021, case fatality rates based on unlinked data increased significantly in Lithuania, the Slovak Republic and the Czech Republic, and case fatality rates based on linked data increased substantially in Türkiye, Lithuania, the Slovak Republic and the Czech Republic (Figure 6.25 and Figure 6.26). During this period, hospital admissions following ischaemic stroke also decreased in most OECD countries. As with heart attack (see section on “Mortality following acute myocardial infarction (AMI)”), a number of studies conducted in OECD countries have found that admitted patients showed higher severity of stroke than in the pre‑pandemic period, owing to delayed hospital arrival time for stroke patients due to emergency medical services processing time – particularly during the initial phase of the pandemic. Close clinical links with COVID‑19 also complicate assessment and monitoring of the resilience of health systems in ensuring access to and quality of acute care.