Many people receiving LTC wish to remain at home for as long as possible, and most countries have increasingly taken steps in recent years to support this preference and promote community and home‑based care. However, depending on individual circumstances, a move to LTC facilities may – at least eventually – be the most appropriate option. For example, people living alone and requiring round-the‑clock care and supervision, or people living in remote areas with limited home care support, may find it difficult to manage at home as their needs increase, and will at some point require LTC services that cannot be delivered at home. It is therefore important that countries retain an appropriate level of residential LTC capacity. The number of beds in LTC facilities and in LTC departments in hospitals offers a measure of the resources available for delivering LTC services to individuals outside their home.
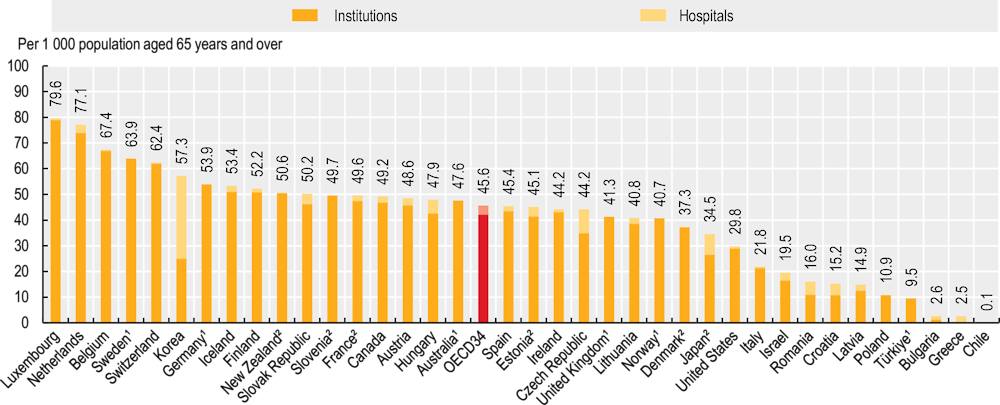
Across OECD countries, there were an average of 46 beds per 1 000 people aged 65 and over in 2021 (Figure 10.21). The vast majority of beds – 42 per 1 000 people aged 65 and over – were located in LTC facilities, while just 4 beds per 1 000 were located in hospitals. The proportion of LTC beds in hospitals exceeded 10% of all LTC beds in just six OECD countries, with Korea (56%), Japan (23%) and the Czech Republic (21%) reporting the highest proportions. Among OECD countries reporting both facility-based and hospital-based LTC beds, the number of beds available per capita varied enormously, with a more than seven‑fold difference between the highest and lowest proportions. Luxembourg, the country with the highest number of beds, reported almost 80 beds per 1 000 people aged 65 and over, compared to almost 11 beds per 1 000 in Poland.
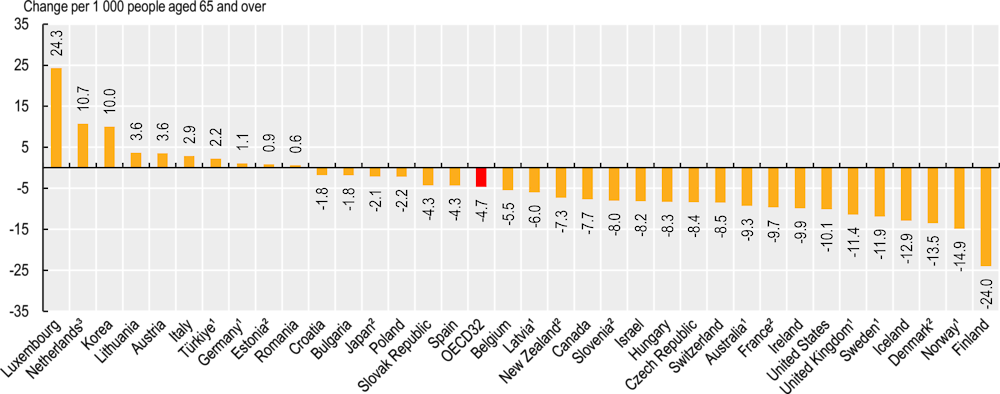
Between 2011 and 2021, OECD countries reduced the number of LTC beds in facilities by an average of 4.7 beds per 1 000 people aged 65 and over (Figure 10.22). In some cases, the number of LTC beds per 1 000 people 65 and over may have fallen even as the absolute number of beds increased, due to population ageing that outpaced the growth in hospital beds. However, the change in the number of beds varied significantly between OECD countries. Over the decade, nine countries reduced the number of LTC beds by about 10 or more, with Finland reducing the number of LTC beds by 24 per 1 000 people aged 65 and over. In contrast, in Luxembourg and Korea the number of LTC beds increased by more than 10 per 1 000 people aged 65 and over between 2011 and 2021. These substantial changes were largely driven by changes in policies over the period. The increase of 10 facility-based LTC beds per 1 000 people aged 65 and over in Korea, for example, came about following the introduction of a public LTC insurance scheme in 2008, while in Sweden, declines (a drop of 11.9 beds per 1 000 people aged 65 and over) were driven by growing home‑based care in ordinary housing, in addition to nursing homes.
Residents of LTC facilities were badly hit during the COVID‑19 pandemic: across 25 OECD countries, more than 40% of COVID‑19 deaths occurred among nursing home residents. Moreover, containment measures – including strict bans on visitation in most countries – dramatically affected the well-being of many residents, even beyond the direct health impact of the virus. Developing and applying models of care that respect the resident’s wishes and promote dignity and autonomy is a critical aspect of high-quality care. This includes ensuring that staff working in LTC facilities are appropriately trained, and that facilities receive the support they need to deliver high-quality care, reduce high turnover and facilitate the recruitment and retention of high-quality care workers (see section on “Long-term care workers”).