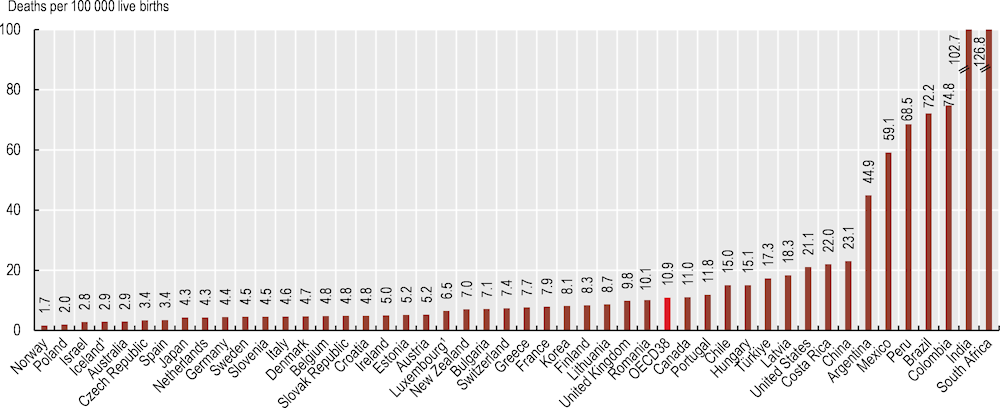
Maternal mortality – the death of a woman during pregnancy or childbirth, or within 42 days of the termination of pregnancy – is an important indicator of a woman’s health status and to assess health system performance. The Sustainable Development Goals set a target of reducing the global maternal mortality ratio to less than 70 deaths per 100 000 live births by 2030 (WHO, 2023[1]).
In OECD countries, the maternal mortality ratio (MMR) averaged 10.9 deaths per 100 000 live births in 2020, which is substantially lower than the target set by the Sustainable Development Goals. Countries including Norway, Poland, Israel, Iceland and Australia had MMRs of fewer than 3 deaths per 100 000 births. However, Colombia is yet to achieve the SDG target, with an MMR of 72 deaths per 100 000 live births in 2020. Mexico also had a significantly high MMR of 55 deaths per 100 000 births. Many OECD accession and partner countries also had high MMRs, ranging from 69 deaths per 100 000 births for Peru to 173 deaths per 100 000 births for Indonesia (Figure 3.17).
Risks of maternal death can be reduced through family planning, better access to high-quality antenatal care, and delivery and postnatal care delivered by skilled health professionals. Addressing disparities in provision of these essential reproductive health services to underserved populations must be included in any strategy. Furthermore, the broad health system strengthening and universal health coverage agenda, along with multisectoral action (including women’s education and tackling violence), are collaborative efforts that are crucial to reducing maternal deaths (WHO et al., 2018[2]).
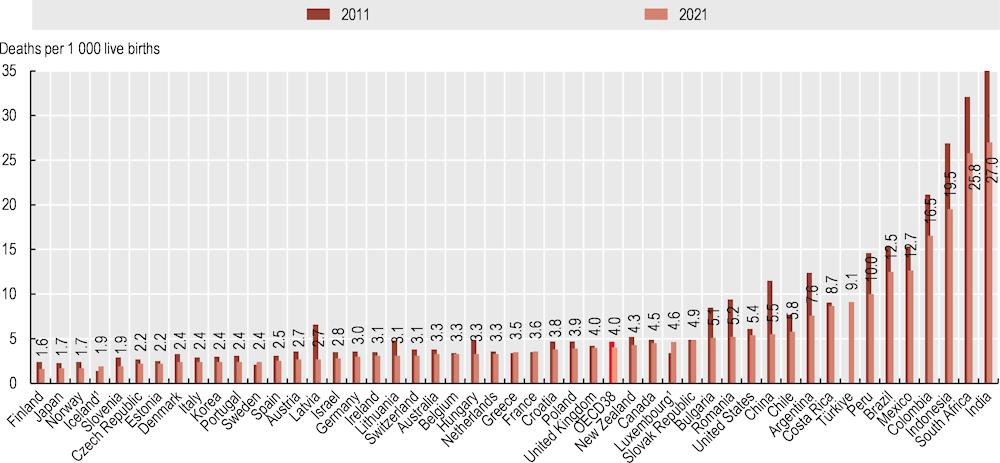
Infant mortality – deaths in children aged less than one year – reflects the impact of economic, social and environmental conditions on the health of mothers and infants, as well as the effectiveness of health systems. Factors such as the education of the mother, quality of antenatal and childbirth care, preterm birth and birth weights, immediate newborn care and infant feeding practices are important determinants of infant mortality.
In 2021, infant mortality was on average at 4 deaths per 1 000 live births in OECD countries, down from 4.7 deaths per 1 000 live births in 2011. Finland, Japan, Norway, Iceland and Slovenia all had infant mortality rates of fewer than 2 deaths per 1 000 live births in 2021. However, infant mortality rates are still relatively high in Colombia (16.5 deaths per 100 000 births) and Mexico (12.7 deaths per 1 000 live births), signalling the correlation that exists between maternal and infant mortality. Among OECD partner countries, infant mortality rates are around 20 deaths or higher per 1 000 live births in India, South Africa and Indonesia – although each of these countries has reduced infant mortality rates considerably since 2011 (Figure 3.18).
Infant mortality can be reduced through cost-effective and appropriate interventions. These include immediate skin-to-skin contact between mothers and newborns after delivery, early and exclusive breastfeeding for the first six months of life, and kangaroo parent care for babies weighing 2 000 g or less. Postnatal care for mothers and newborns within 48 hours of birth, delayed bathing until after 24 hours of childbirth, and dry cord care are important in reducing infant deaths. Management and treatment of neonatal infections, pneumonia, diarrhoea, and malaria are also critical.