Climate change is one of the biggest challenges for present and future generations. It is linked to many different types of environment distress, including air pollution and extreme temperatures. Air pollution is already the most significant environmental health risk and a major cause of death and disability, and its future impact is likely to be even greater without adequate policy action. Projections have estimated that outdoor air pollution may cause between 6 million and 9 million premature deaths a year worldwide by 2060, and cost 1% of global gross domestic product (GDP) as a result of sick days, medical bills and reduced agricultural output (OECD, 2015[1]).
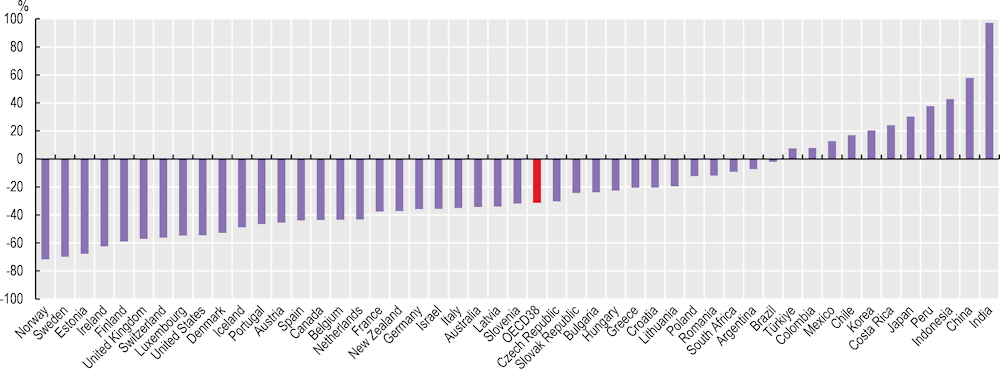
Among OECD countries, premature deaths from ambient (outdoor) particulate matter pollution – and especially fine particulate matter (PM2.5) declined by about 31% between 2000 and 2019, from 42 deaths per 100 000 people in 2000 to about 29 deaths per 100 000 in 2019 (Figure 4.15). Over the same period, average population exposure to ambient particulate matter declined by 32% on average across OECD countries. While mortality associated with ambient particulate matter pollution fell in most OECD countries, it increased between 2000 and 2019 in seven: Japan, Costa Rica, Korea, Chile, Mexico, Colombia and Türkiye, including an increase of 20% or more in Japan (30%), Costa Rica (24%) and Korea (20%). Mortality associated with ambient particulate matter pollution fell by more than 50% in ten OECD countries, with the greatest reductions in Norway (72%) and Sweden (70%). While policies to reduce pollution have led to some important reductions in deaths caused by air pollution, they remain a major public health and environmental concern.
Extreme temperatures are also a consequence of climate change. Both extreme heat and extreme cold can cause health problems and lead to death. For OECD countries, extreme cold has generally had a greater impact on mortality than heatwaves – particularly in Central and Eastern Europe and the Nordic countries – although heatwaves have also caused significant numbers of deaths in certain years. The record-warm summer of 2003, for example, caused around 80 000 deaths in Europe, and the heatwaves in the summer of 2015 caused more than 3 000 deaths in France alone. Furthermore, the 2021 heatwave in Western Canada and the United States caused hundreds of deaths, especially among older adults.
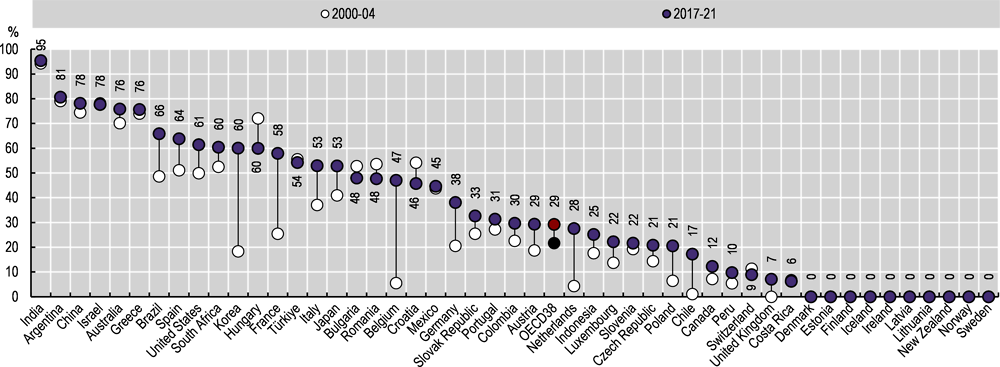
On average across the 38 OECD countries, the proportion of the population estimated to have been exposed to hot summer days increased from 22% on average from 2000‑04, to 29% on average in 2017‑21 – a 35% increase across the two periods (Figure 4.16). In ten countries – Chile, Belgium, the Netherlands, Korea, Poland, France, Germany, Canada, Luxembourg and Austria – the proportion of the population who were exposed to hot summer days increased by over 50%, including six countries (Chile, Belgium, the Netherlands, Korea, Poland and France) in which the proportion more than doubled between 2000‑04 and 2017‑21. In the United Kingdom, the proportion increased from 0% to 7% between the two periods. Increased exposure to hot weather has already led to increases in mortality, with further heat-related deaths and morbidity likely to arise as temperatures continue to increase. Globally, heat-related deaths among older populations (aged 65 and older) are estimated to have risen by more than two‑thirds (68%) between 2000‑04 and 2017‑21 (Romanello et al., 2022[2]).
Inter-sectoral policies are needed to address the impact of climate change. Countries can start planning to address pollution and its impacts on health, for instance, by creating partnerships with international, national and local stakeholders, including local city authorities and ministries of industry, environment, transport and agriculture. Reducing crop burning and lowering emissions from motor vehicles and industries would lower ambient air pollution. Health systems can also contribute, by preparing for new diseases that can develop with new climate and biodiversity conditions; promoting consumption of sustainably grown and sourced food; and reducing the carbon footprint of health facilities. In addition, health providers can reduce the environmental footprint in hospitals and in nursing homes by encouraging healthier food consumption, waste reduction and efficient energy use (OECD, 2017[3]).