OECD populations are ageing rapidly. The demand on the LTC sector to provide care for more, and older, people with complex conditions and heightened needs for expert care is increasing as a result. This puts an enormous strain on LTC systems – a strain that is projected to increase in the coming years as OECD populations continue to age (see section on “Demographic trends”).
LTC entails safety risks, which were made evident by the rapid spread of COVID‑19 among residents and health workers in LTC settings. The advanced age of many residents, lack of sufficient personal protective equipment, and poor infection control meant that many LTC facilities experienced outbreaks that spread rapidly (OECD, 2020[1]). Another significant concern for LTC safety is healthcare‑acquired infections with antibiotic-resistant bacteria, which can lead to infections that are difficult or even impossible to treat (see section on “Major public health threats” in Chapter 3). These infections are also generally considered to be preventable through standard prevention and hygiene measures. Safety risks amongst people in LTC facilities due to medicines also exist, as is the case with benzodiazepines and polypharmacy more in general.
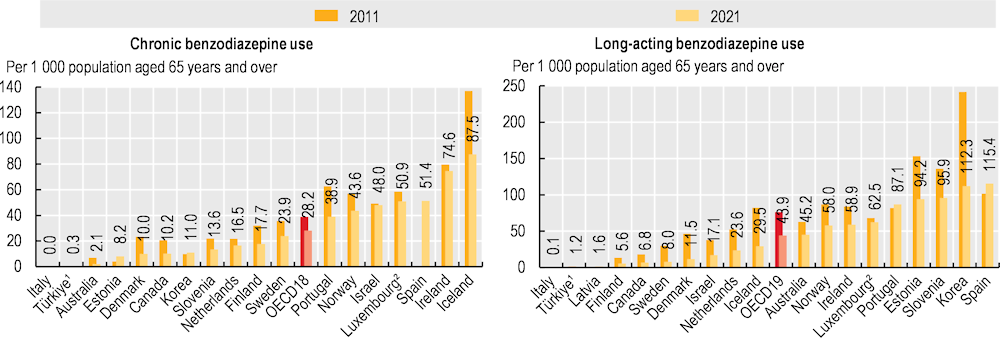
For older people, most guidelines advise complete avoidance (that is, an ideal rate of 0%) of benzodiazepines because of the associated risks of dizziness, confusion and falls. Even so, benzodiazepines continue to be prescribed for older adults for anxiety and sleep disorders. Long-term use of benzodiazepines can lead to adverse events (overdoses), tolerance, dependence, and dose escalation. Long-acting (as opposed to short-acting) benzodiazepines are furthermore discouraged for use in older adults because they take longer for the body to eliminate (OECD, 2017[2]).
Use of benzodiazepines varies greatly, but – on average – declined between 2011 and 2021 in OECD countries. Chronic use of benzodiazepines across OECD countries fell from 39 patients per 1 000 population aged 65 and over in 2011, to 28.2 per 1 000 in 2021, on average. Figures ranged from below 1 patient per 1 000 population aged 65 and over in Italy and Türkiye to 87.5 per 1 000 in Iceland. For long-acting benzodiazepines, the OECD average figure fell from 76 patients per 1 000 population aged 65 and over in 2011, to almost 44 per 1 000 in 2021. Rates were again relatively low in Italy and Türkiye, and also Latvia, at less than 2 patients per 1 000 population aged 65 and over, whereas in Spain and Korea rates were above 110 per 1 000 (Figure 10.10). The largest declines in chronic use occurred in Australia, Denmark, and Canada, while Sweden, Denmark and Iceland experienced the largest decline in use of long-acting benzodiazepines. The wide variation is explained in part by different reimbursement and prescribing policies for benzodiazepines, as well as by differences in disease prevalence and treatment guidelines.
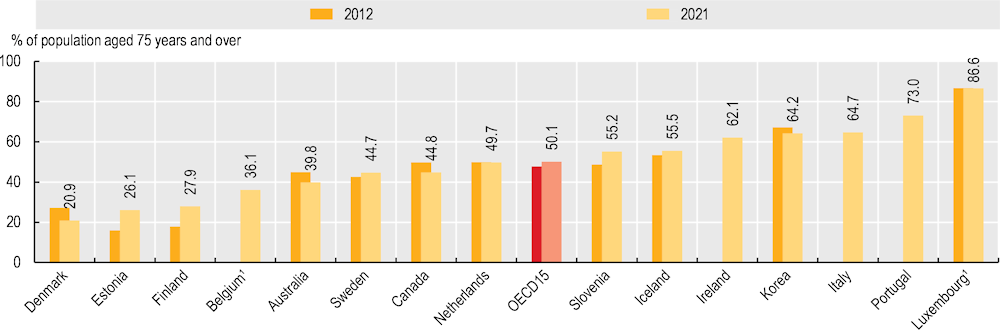
Ageing and multimorbidity often require older patients to take multiple medicines (polypharmacy) for long periods of their lives. While polypharmacy is in many cases justified for the management of multiple conditions, inappropriate polypharmacy increases the risk of adverse drug events, medication error and harm – resulting in falls, episodes of confusion and delirium.
Across a selection of 15 OECD countries with broader data coverage, the proportion of adults aged 75 and over taking at least five medications at the same time increased from 47.7% of the population in 2012 to 50.1% in 2021. Countries such as Denmark, Estonia and Finland reported the lowest rates in 2021, at less than 28%, while Luxembourg reported the highest rates at 86.6%, followed by Portugal, Italy, Korea and Ireland at more than 62% (Figure 10.11). These large variations are explained in part by the establishment of targeted polypharmacy initiatives in some countries, including related reimbursement and prescribing policies. Over time, Denmark, Australia and Canada have seen a decrease of 10% or more in the proportion of adults aged 75 and over taking at least five medications at the same time (which corresponds to a reduction of between 5 and 6 percentage points), while Estonia had an increase of 63.1% and Finland an increase of 56.7% (both increased by 10.1 percentage points). Slovenia, Sweden and Iceland also exhibited an increase in polypharmacy.