Mortality due to coronary heart disease has declined substantially over recent decades (see section on “Mortality from circulatory diseases” in Chapter 3). Reductions in smoking (see section on “Smoking” in Chapter 4) and improvements in treatment for heart diseases have contributed to this decline (OECD, 2015[1]). Despite this progress, AMI (heart attack) remains one of the leading causes of death and the main cause of cardiovascular death in many OECD countries, highlighting the need for further reductions in risk factors and care quality improvements (OECD/The King's Fund, 2020[2]).
Metrics of 30‑day mortality after hospital admission for AMI are reflective of processes of care, such as timely transport of patients and effective medical interventions. As such, the indicator is influenced not only by the quality of care provided in hospitals but also by differences in the patterns of hospital transfers, length of stay and AMI severity across countries.
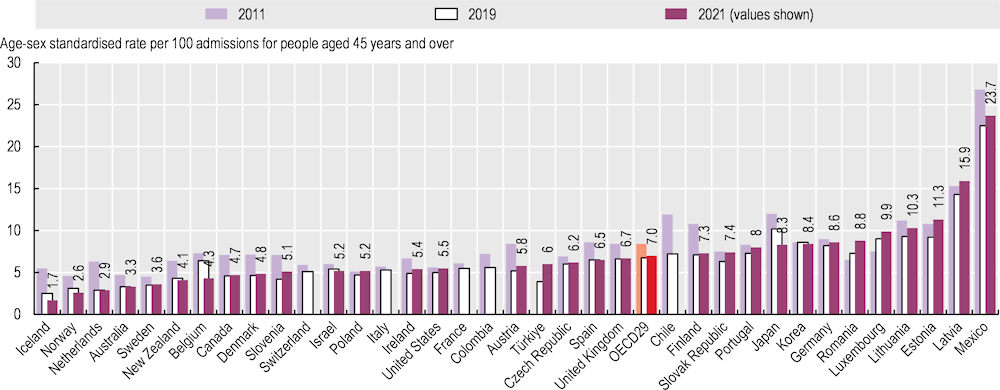
Figure 6.23 shows mortality rates within 30 days of admission to hospital for AMI using unlinked data – that is, only counting deaths that occurred in the hospital where the patient was initially admitted – among patients aged 45 and over. The lowest rates in 2021 were in Iceland, Norway, the Netherlands, Australia and Sweden (less than 4%) while the highest rates were in Latvia (15.9%) and Mexico (23.7%). In Mexico, many hospitals lack the capacity to perform AMI diagnosis, and pharmacological and mechanical reperfusion (Pérez-Cuevas et al., 2020[3]), and this might be associated with high AMI mortality rates.
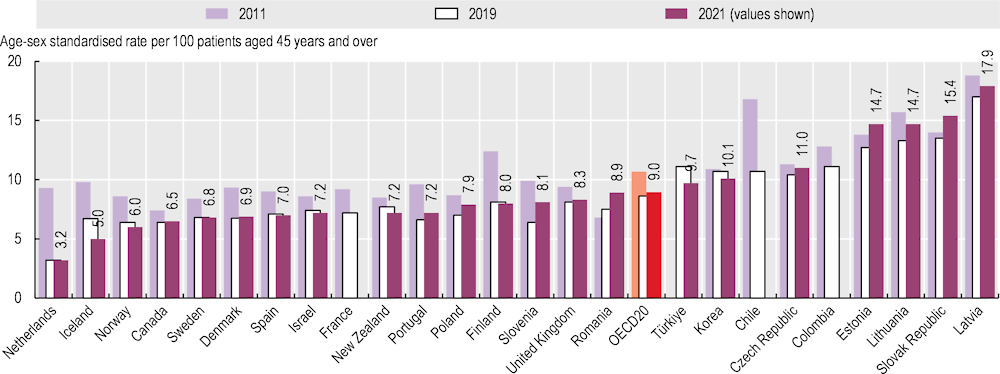
Figure 6.24 shows the same 30‑day mortality rate but calculated based on linked data, whereby the deaths are recorded regardless of where they occurred after hospital admission (in the hospital where the patient was initially admitted, after transfer to another hospital or after being discharged). Based on these linked data, AMI mortality rates in 2021 ranged from 3.2% in the Netherlands to 17.9% in Latvia.
Case fatality rates for AMI decreased substantially between 2011 and 2019. Across OECD countries, the average rate fell from 8.4% to 6.7% for same‑hospital deaths (Figure 6.23) and from 10.7% to 8.6% for deaths in and out of hospital (Figure 6.24), and this is reflected in a decrease in rates of overall mortality due to AMI over the same period.
Between 2019 and 2021, however, the average rate increased by 4% for both same‑hospital deaths and deaths in and out of hospital. The increase was significantly high in Türkiye and Germany for same‑hospital deaths and a substantial increase was also observed for deaths in and out of hospital in the Slovak Republic and Poland. A number of subnational studies in OECD countries point out that, during the pandemic, the average severity of AMI patients admitted to hospital increased due to hesitancy in seeking care – particularly among those with milder conditions – and the time from the onset of symptoms to treatment was prolonged due to later patient presentations at hospitals and longer processing time at hospital before initiating a needed procedure. A mix of these factors may have contributed to an increase in 30‑day mortality rates during the pandemic.
Cross-country analysis of recent 30‑day case fatality trends is also challenging because people with underlying cardiovascular conditions tend to be more vulnerable to dying from COVID‑19 infection, while at the same time COVID‑19 infection itself is associated with an increased risk of different types of cardiovascular disease – both ischaemic heart disease and cerebrovascular diseases. Therefore, COVID‑19 prevalence may also have affected changes in mortality rates due to diseases of the circulatory system, with close clinical links with COVID‑19 complicating the cause of death coding across countries.
More data and analyses are needed to assess cross-country variations in accessibility and quality of acute care provided to patients with acute cardiovascular events such as AMI during the pandemic. While timely provision of high-quality care is required from the onset of the disease among these patients, 30‑day mortality rates only capture the quality of care provided once admitted to hospital. Pre‑hospital access to healthcare such as emergency medical services, which is also crucial for outcomes of AMI patients, is not well understood.