Consultations with primary care doctors are for many people the most frequent contact with health services, and often provide an entry point for subsequent medical treatment. Consultations take place in doctors’ clinics, community health centres, hospital outpatient departments or, in some cases, patients’ own homes. Increasingly, teleconsultations are offered to patients, whereby consultations take place online, often through video calls (OECD, 2023[1]).
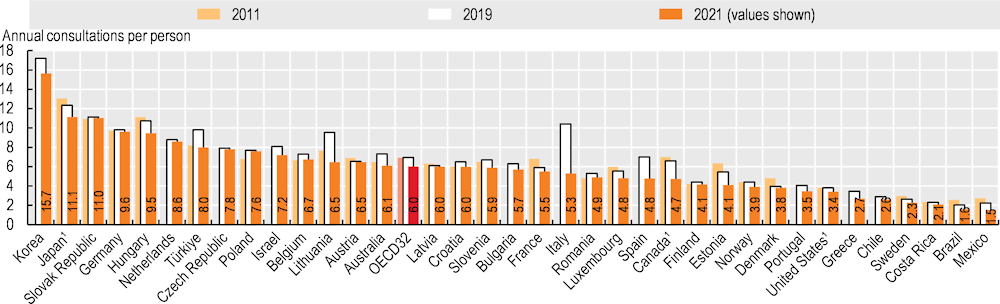
In 2021, the average number of annual in-person doctor consultations per person among OECD countries ranged from fewer than 3 in Mexico, Costa Rica, Sweden, Chile and Greece to over 15 in Korea (Figure 5.11). The OECD average was 6 consultations per person per year, with most countries reporting between 4 and 10. Differences in service delivery modalities explain some of the cross-country variation. In Canada, Finland, Sweden, the United Kingdom and the United States, the relatively low number of consultations can be explained in part by the enhanced role that nurses and other health professionals play in primary care – notably in management of patients with chronic diseases and in dealing with patients with minor health issues. This lessens the need for doctor consultations (Maier, Aiken and Busse, 2017[2]). In recent years, teleconsultations have also played a greater role in many countries.
Provider payment methods and levels of co-payments also have an impact on the number of doctor consultations. In some countries, doctors are paid predominantly by fee‑for-service (as in Germany, Japan, Korea and the Slovak Republic). Such countries tend to have higher consultation rates than those countries where doctors are mainly paid by salaries or capitation (such as Denmark, Finland, Mexico and Sweden). However, in the United States, doctors are paid mainly by fee‑for-service, but consultation rates are below average. This may reflect the high co-payments a large proportion of the population face, which can cause patients to not consult a doctor because of the cost of care.
The number and type of doctor consultations can vary among different socio‑economic groups. Wealthier individuals are more likely to see a doctor than individuals in the lowest income quintile, for a comparable level of need. Income inequalities in accessing doctors are much more marked for specialists than for GP consultations (OECD, 2019[3]).
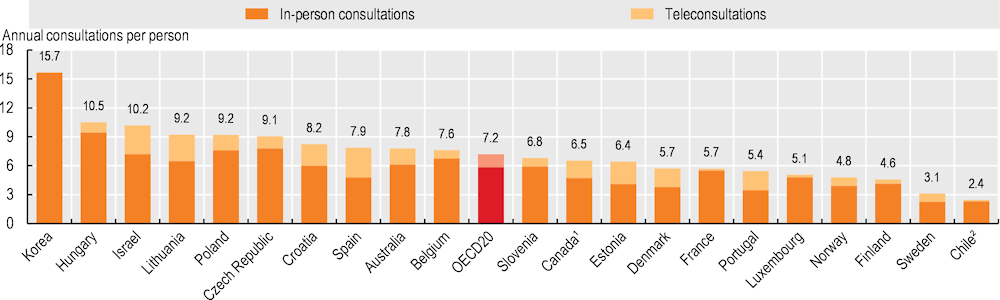
While in-person doctor consultations were relatively stable in most OECD countries between 2011 and 2019 (except for large increases in Türkiye and Lithuania), in-person consultations were lower in 2021 than 2019 in all countries. This reflects the substantial impact of COVID‑19 in terms of disruption to services and people’s reluctance to visit healthcare facilities due to concerns about catching the virus. It also reflects an increased use of teleconsultations during the pandemic in all countries with available data (see section on “Digital health”). Indeed, 19% of all doctor consultations were teleconsultations in 2021, on average across 20 OECD countries with comparable data (Figure 5.12). In Spain, Portugal, Estonia and Denmark, teleconsultations were particularly important, comprising over 30% of all doctor consultations.
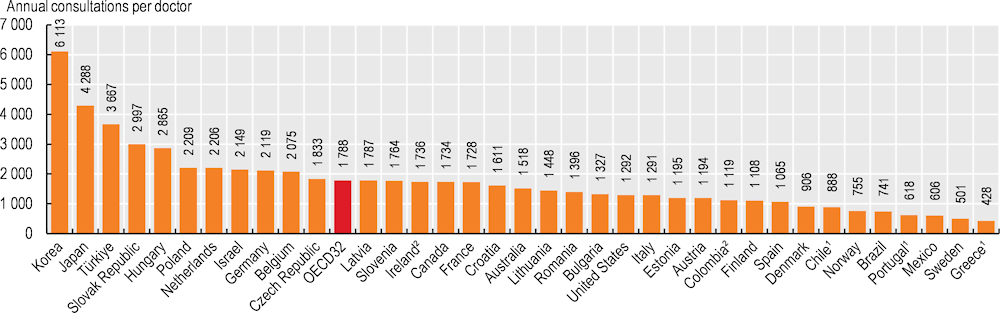
Information on the number of doctor consultations per person can be used to estimate the annual number of consultations per doctor (in-person). This indicator should not be taken as a measure of doctors’ productivity, since consultations vary in length and effectiveness, and because it excludes services doctors deliver for hospital inpatients, as well as time spent on research and administration. Keeping these comparability issues in mind, the estimated number of consultations per doctor is highest in Korea, Japan and Türkiye (Figure 5.13). Numbers were lowest in Greece and Sweden. In Sweden, consultations with doctors in both primary care and hospital settings tend to be focused on patients with more severe and complex cases.