When patients with chronic conditions require care from multiple providers across different healthcare settings, fragmented care can lead to poor health outcomes, unmet needs, and excessive service utilisation and costs. Recognising the need for care integration, countries are developing new models of care, aiming to enhance population health, improve patient experiences, reduce healthcare costs, support the well-being of healthcare professionals and promote health equity (OECD, 2023[1]).
Optimal integration between different levels of care for stroke and congestive heart failure (CHF) patients minimises unnecessary readmissions to hospitals and reduces mortality, while maximising appropriate prescriptions (Barrenho et al., 2022[2]). For patients with stroke and CHF discharged from hospital, outcomes such as readmission, mortality and compliance with prescription guidelines can measure the performance of health systems in delivering integrated care.
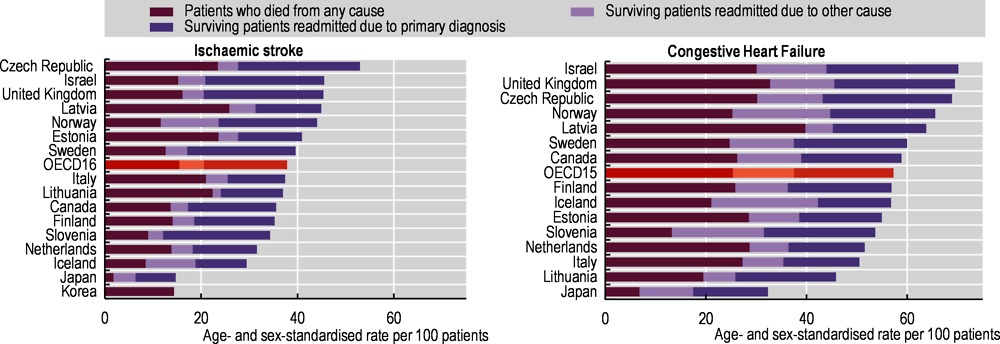
Figure 6.33 shows the proportion of patients with adverse outcomes within a year after discharge for ischaemic stroke and CHF in 2021. For patients discharged after a stroke, on average, 16% of the patient cohort died, while 22% were readmitted. Iceland (30%) and the Netherlands (32%) reported the lowest rates of adverse outcomes – both mortality and readmissions – and they also reported among the lowest rate for each adverse outcome. The highest overall adverse outcome rate was reported in the Czech Republic (53%). For CHF, Lithuania had the lowest rate of overall adverse outcomes (46%); this may reflect recent policy focus on digital health, which facilitated exchanges of medical records, care co‑ordination and prevention at the primary level (OECD, 2018[3]), although care integration still has room for improvement. On the other hand, in Israel, 70% of CHF patients had an adverse event, with rates also above the OECD averages for mortality and readmissions separately.
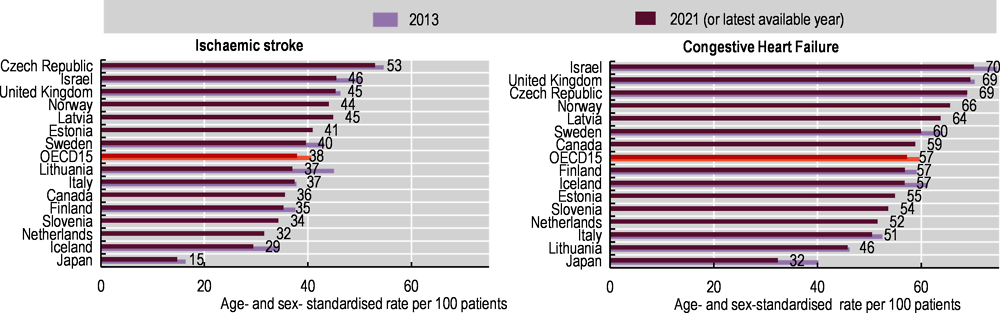
Figure 6.34 shows that in all countries with available data the proportion of stroke or CHF patients who died or were readmitted within a year after discharge decreased in recent years. Between 2013 and 2021, the average rate decreased by 7% for stroke and about 4% for CHF across OECD countries. The largest decreases in this period were observed in Lithuania (by 18%) for stroke and in Japan (by 20%) for CHF. In most countries, the proportion of patients with adverse outcomes was stable during the pandemic.
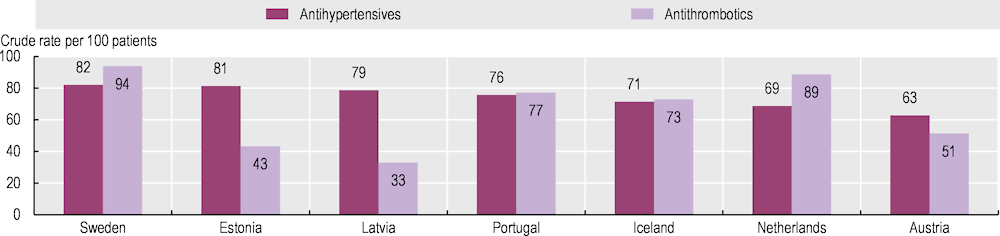
Ischaemic stroke patients should receive antihypertensive and antithrombotic prescriptions for secondary prevention after hospital discharge. Having at least one prescription of these medicines in the 18 months after discharge provides insight into the quality of integration between hospital and community care (Barrenho et al., 2022[2]). Figure 6.35 shows that the prescription rate for antihypertensives varied from 63% in Austria to 82% in Sweden, while the prescription rate for antithrombotics ranged from 33% in Latvia to 94% in Sweden. The outstanding Swedish performance can be explained by adequate information transfers between levels of care and diagnosis recording (Dahlgren et al., 2017[4]).