Alcohol use is a leading cause of death and disability worldwide, particularly among those of working age. High alcohol intake is a major risk factor for heart diseases and strokes, liver cirrhosis and certain cancers, but even low and moderate alcohol consumption increases the long-term risk of these diseases. Alcohol also contributes to more car crashes and injuries, violence, homicides, suicides and mental health disorders than any other psychoactive substance, particularly among young people. Alcohol-related diseases and injuries incur a high cost to society. An average of 2.4% of health expenditure is spent on dealing with the harm caused by alcohol consumption, and the figure reaches as high as 4% in some countries (OECD, 2021[1]).
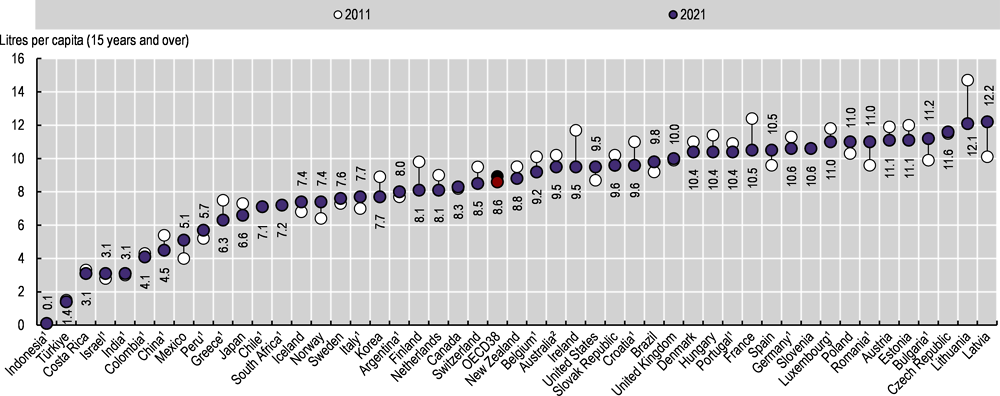
Measured through sales data, overall alcohol consumption averaged 8.6 litres per person across OECD countries in 2021, down from 8.9 litres in 2011 (Figure 4.4). Latvia and Lithuania reported the highest consumption in 2021 (over 12 litres per person), followed by the Czech Republic, Estonia and Austria – all with over 11 litres per person. Türkiye, Costa Rica, Israel and Colombia had comparatively low consumption levels (under 5 litres per person). Among accession and partner countries, consumption was relatively high in Bulgaria and Romania (11 litres and over per person) and low in Indonesia, India and China (under 5 litres). Average consumption fell in 23 OECD countries between 2011 and 2021, with the largest reductions in Lithuania and Ireland (by more than 2 litres). However, alcohol consumption increased by more than 2 litres per person in Latvia, and by about 1 litre per person in Mexico and Norway, as well as in accession countries Bulgaria and Romania.
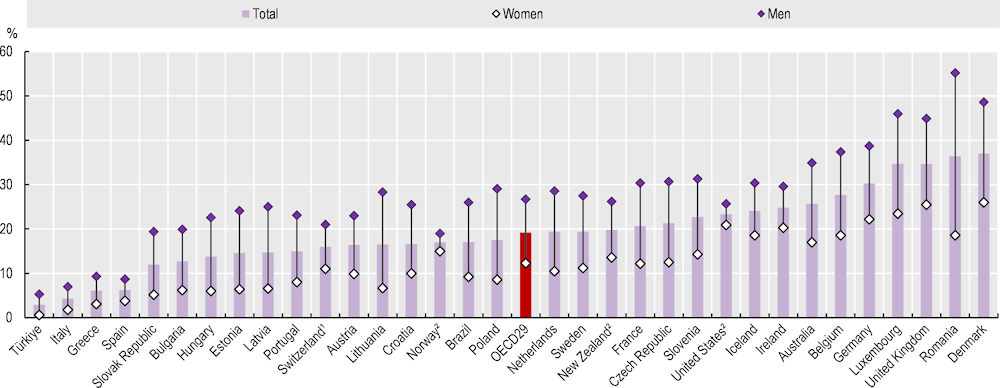
While national data on overall consumption per capita facilitate the assessment of long-term trends, they do not identify harmful drinking patterns, such as heavy episodic drinking (also called binge drinking). Nearly one in five adults (19%) reported heavy episodic drinking at least once a month, on average across 29 OECD countries in 2019 (Figure 4.5). This proportion varies 10‑fold, from less than 3% in Türkiye and Italy to more than 30% in Germany, Luxembourg, the United Kingdom and Denmark, as well as Romania. The data presented herein may differ from estimates derived from other national sources. In all countries, men were more likely than women to report heavy episodic drinking. On average across OECD countries, 26% of men reported heavy episodic drinking at least once a month compared to 12% of women.
Policies to tackle harmful alcohol use include broad-based strategies and those that target heavy drinkers. Comprehensive policy packages built on a “PPPP strategy” – pricing policies to limit affordability of cheap alcohol, policing to counter drink-driving, primary care‑based counselling for people with harmful patterns of alcohol use, and protecting children from alcohol promotion – are highly cost-effective in tackling harmful alcohol use (OECD, 2021[1]). Two recent innovative changes are emerging in the alcohol policy landscape. One is the use of minimum unit pricing (MUP), which sets a floor price beneath which alcohol cannot be sold legally. MUP targets cheap alcohol that is consumed by heavy drinkers. MUP was introduced in Ireland in 2022, and is already in place in two of the United Kingdom nations (Scotland and Wales), and in some regions in Australia and Canada. The second innovation is legislation mandating the labelling of alcohol products. While warning labels about the dangers of drinking while pregnant already exist in some countries, Ireland became the first country globally to mandate labels with population-wide health warnings on alcohol products (such as alcohol-associated risk of cancers and liver diseases).