Cancer was the second leading cause of death in OECD countries after circulatory diseases, accounting for 21% of all deaths in 2021. Leading causes of cancer-related mortality included lung cancer (20%), colorectal cancer (10.9%), breast cancer (14.7% among women) and prostate cancer (10.1% among men). These four represent almost 44% of all cancers diagnosed in OECD countries. Mortality rates from cancer have fallen in all OECD countries since 2000, although on average the decline has been more modest than for circulatory diseases.
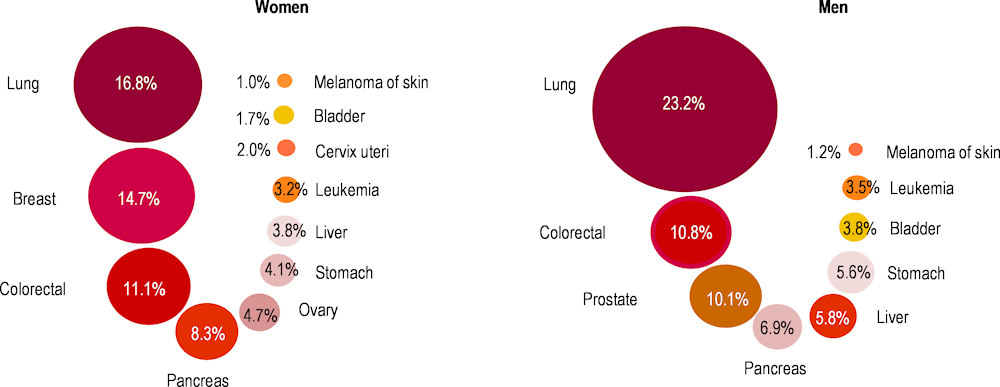
Lung cancer is the main cause of death for both men and women, accounting for 23.2% of cancer deaths among men and 16.8% among women (Figure 3.13). Smoking represents the main risk factor for lung cancer. Colorectal cancer is also a major cause of death for both men and women, representing 10.9% of cancer-related deaths for both sexes. Widespread screening programmes for colorectal cancers for older populations have led to declining incidence among older adults. In recent years, however, many OECD countries have observed rising incidence of colorectal cancer among younger patients. Apart from age and genetic factors, exposure to ultraviolet radiation, a diet high in fat and low in fibre, lack of physical activity, obesity, smoking and alcohol consumption all increase the risk of developing the illness.
Breast cancer is the second most common cause of cancer mortality in women (14.7% of deaths). While incidence rates for breast cancer have increased over the past decade, mortality rates have declined or stabilised – indicative of earlier diagnosis and treatment – and consequently survival rates are higher (see section on “Cancer screening” in Chapter 6). Prostate cancer is the third most common cause of cancer mortality among men, accounting for 10.1% of all cancer-related deaths.
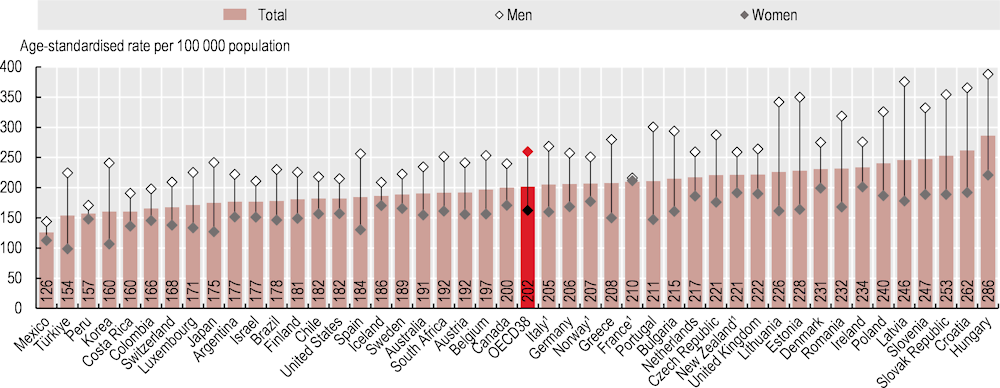
Mortality rates from cancer averaged 202 deaths per 100 000 people across OECD countries in 2021, up from 191 in 2019 (Figure 3.14). Among OECD countries, mortality rates were highest in Hungary, the Slovak Republic, Slovenia, Latvia and Poland (240 or above) and lowest in Mexico and Türkiye (fewer than 160).
Earlier diagnosis and treatment significantly increase cancer survival rates. This partly explains why, for example, countries such as Australia and Belgium have below-average mortality rates despite having relatively high rates of cancer incidence. Analysis of survival following cancer for 2010‑14 found that both Australia and Belgium had higher than average five‑year net survival for common cancers (OECD, 2023[1]; OECD, 2021[2]).
The COVID‑19 pandemic severely disrupted programmes for cancer diagnosis and treatment across OECD countries. The numbers of cancer screening and treatment services were significantly diminished in almost all OECD countries, particularly during the onset of the pandemic and the first rollout of restrictions and lockdowns after March 2020. As a result, diagnosis and treatment of cancer were considerably delayed in early 2020 across most OECD countries (OECD, 2023[3]).
Cancer incidence rates have historically been higher for men than women in OECD member and partner countries. Cancer mortality rates are higher for men in all OECD member countries. The gap is widest in Latvia, Estonia and Lithuania, where cancer mortality is 2.1 times higher for men, while in France male mortality is only 2% higher than female mortality (Figure 3.14). Greater prevalence of risk factors among men – notably smoking and alcohol consumption – drive much of this gender gap in cancer incidence and mortality. Additionally, interventions to reduce socio‑economic inequalities in cancer mortality should focus on people with lower levels of education, as this population group has higher cancer mortality rates across most OECD countries (OECD, 2023[3]).